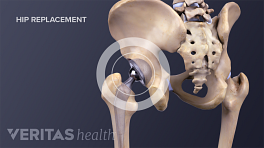
The medical field is continually evolving and trying to improve outcomes for people who get hip replacements. In the meantime, patients and doctors must make choices based on the information currently available. The bullet points below summarize much of what we know about the pros and cons of anterior hip replacement surgery.
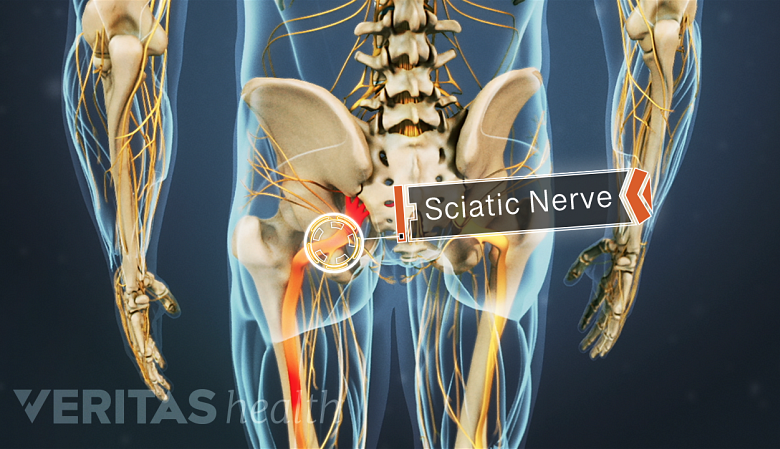
Limited research suggests the anterior approach poses less risk to the sciatic nerve, which is located in the posterior of the leg.
In This Article:
- All About Anterior Hip Replacement
- Anterior vs. Posterior Hip Replacement Surgeries
- Advantages and Disadvantages of Anterior Hip Replacement
- Deciding to Have an Anterior Hip Replacement
Potential Advantages of Anterior Hip Replacement
Proponents of anterior hip replacement surgery believe it offers several advantages, including:
Less damage to major muscles
The anterior approach avoids cutting major muscles. There are fewer muscles at the front of the hip, and the surgeon works between them, rather than cutting through muscle fibers or detaching muscles from bones (and then having to make repairs at the end of the surgery).
Less post-operative pain
Because the surgery does not require cutting major muscles, patients typically experience less pain after surgery and require less pain medication.
Faster recovery
Research suggests people who have anterior hip replacements stop using walkers, canes, and other assistive devices 5 to 7 days sooner than traditional hip surgery patients.
1
Taunton MJ, Mason JB, Odum SM, Springer BD. Direct Anterior Total Hip Arthroplasty Yields More Rapid Voluntary Cessation of All Walking Aids: A Prospective, Randomized Clinical Trial. J Arthroplasty. 2014 May 25. pii: S0883-5403(14)00340-4. doi: 10.1016/j.arth.2014.03.051. [Epub ahead of print] PubMed PMID: 25007723.
See Total Hip Replacement Surgery Recovery
Fewer postsurgical precautions
After hip replacement surgery, patients are given a list of precautions—certain movements and activities that should be avoided in order to prevent the new hip from dislocation. (Precautions are typically followed for the first 6 weeks after surgery.)
Anterior approach surgeons tend to assign fewer or no postsurgical precautions. However, there is no clear consensus on this issue since some surgeons performing traditional hip replacement are also forgoing the post-operative hip precautions.
While anterior hip replacement may offer some advantages, there are also potential limitations or disadvantages.
Potential Disadvantages of Anterior Hip Replacement
Anterior hip replacement does have a few limitations:
There may be wound healing issues
Research suggests that people who undergo anterior hip replacement may be more likely to have a problem with wound healing, particularly infection. For example, a study of 505 anterior hip replacements and 1288 posterior hip replacements found that 7 (1.4%) of the anterior hip patients had wound healing problems compared to 5 (0.2%) of the posterior patients.
2
Christensen CP, Karthikeyan T, Jacobs CA. Greater prevalence of wound complications requiring reoperation with direct anterior approach total hip arthroplasty. J Arthroplasty. 2014 Sep;29(9):1839-41. Epub 2014 May 2.
While wound-healing issues are usually mild and self-limiting (meaning they typically resolve over time even without medical treatment), some may involve an infection of the new hip joint, which is a serious concern.
Obese or very muscular people may not be good candidates
Depending on the surgeon's experience, this surgery may not be appropriate for obese or very muscular patients, because the additional soft tissue can make it difficult for the surgeon to access the hip joint.
It is a technically demanding surgery
Surgeons face a steep learning curve for this procedure. The anterior incision provides a restricted view of the hip joint, making it a technically demanding procedure.
See Total Hip Replacement Surgical Procedure
It is important to remember that a successful hip replacement surgery depends on many factors besides the surgical approach. For example, the knowledge and skill of the surgeon, the type of hip prosthesis used, the patient's weight and build, and the ability and willingness of the patient to participate in surgical preparation and post-surgical rehabilitation are important factors.
Similar Dislocation Rates for Anterior and Posterior Surgeries
For many years, experts believed that people who underwent anterior hip replacement surgery had a lower rate of hip dislocation than patients who underwent lateral or posterior hip replacement surgeries. Research now suggests that anterior hip replacement has a similar rate of dislocation as posterior hip replacement, and it may have a higher rate of dislocation than lateral hip replacement. 3 Aggarwal VK, Iorio R, Zuckerman JD, and Long WM. Surgical Approaches for Primary Total Hip Arthroplasty from Charnley to Now: The Quest for the Best Approach. JBJS Reviews. January 2020; 8 (1): e0058. DOI 10.2106/JBJS.RVW.19.00058
Similar Potential for Nerve Damage
There is a potential risk of nerve injury with any type of hip replacement approach. In anterior hip replacement, the surgical area is located near the lateral cutaneous femoral nerve, which runs down the front of the pelvis and past the hip to supply sensation to the outer thigh (it does not affect muscle control or strength).
Following anterior hip replacement surgery, there is potential for numbness in the thigh, and, in rare cases, a painful irritation of the skin supplied by that nerve, known as meralgia paresthetica. This condition is rare and happens in less than 1% of patients. 4 Post, ZD, Orozco F, Diaz-Ledezma C, Hozack WJ, and Ong A. Direct anterior approach for total hip arthroplasty: indications, technique, and results. Journal of the American Academy of Orthopaedic Surgeons. 2014;22:595-603.
While research is limited, many studies seem to suggest that the risk of damage to the major nerves near the hip, in particular the sciatic nerve, is lower with the anterior approach than with the traditional approaches. 5 Kennon RE, Keggi JM, et al. Total hip arthroplasty through a minimally invasive anterior surgical approach. Journal of Bone and Joint Surgery. 2013;85-A:39-48. , 6 Berend KR, Lombardi, AV, et al. Enhanced early outcomes with the anterior supine intermuscular approach in primary total hip arthroplasty. Journal of Bone and Joint Surgery. 2009;91 Supple:107-20. , 7 Matta JM et al. Single-incision anterior approach for total hip arthroplasty on an orthopaedic table. Clinical Orthopaedics and Related Research. 2005;441:115 This is because the sciatic nerve runs behind the hip joint, so it is not exposed when using the anterior approach.
A patient considering anterior hip replacement surgery should speak with his or her surgeon about potential advantages and disadvantages in the context of the individual's specific circumstances, such as the patient’s hip arthritis, anatomy, overall health, and lifestyle.
See Indications and Eligibility for Total Hip Replacement Surgery
- 1 Taunton MJ, Mason JB, Odum SM, Springer BD. Direct Anterior Total Hip Arthroplasty Yields More Rapid Voluntary Cessation of All Walking Aids: A Prospective, Randomized Clinical Trial. J Arthroplasty. 2014 May 25. pii: S0883-5403(14)00340-4. doi: 10.1016/j.arth.2014.03.051. [Epub ahead of print] PubMed PMID: 25007723.
- 2 Christensen CP, Karthikeyan T, Jacobs CA. Greater prevalence of wound complications requiring reoperation with direct anterior approach total hip arthroplasty. J Arthroplasty. 2014 Sep;29(9):1839-41. Epub 2014 May 2.
- 3 Aggarwal VK, Iorio R, Zuckerman JD, and Long WM. Surgical Approaches for Primary Total Hip Arthroplasty from Charnley to Now: The Quest for the Best Approach. JBJS Reviews. January 2020; 8 (1): e0058. DOI 10.2106/JBJS.RVW.19.00058
- 4 Post, ZD, Orozco F, Diaz-Ledezma C, Hozack WJ, and Ong A. Direct anterior approach for total hip arthroplasty: indications, technique, and results. Journal of the American Academy of Orthopaedic Surgeons. 2014;22:595-603.
- 5 Kennon RE, Keggi JM, et al. Total hip arthroplasty through a minimally invasive anterior surgical approach. Journal of Bone and Joint Surgery. 2013;85-A:39-48.
- 6 Berend KR, Lombardi, AV, et al. Enhanced early outcomes with the anterior supine intermuscular approach in primary total hip arthroplasty. Journal of Bone and Joint Surgery. 2009;91 Supple:107-20.
- 7 Matta JM et al. Single-incision anterior approach for total hip arthroplasty on an orthopaedic table. Clinical Orthopaedics and Related Research. 2005;441:115