The most concerning complications related to hip replacement are those that threaten the overall health and life of the patient, such as complications involving anesthesia. Other complications, such as differences in leg length, are not medically serious but can affect comfort and quality of life.
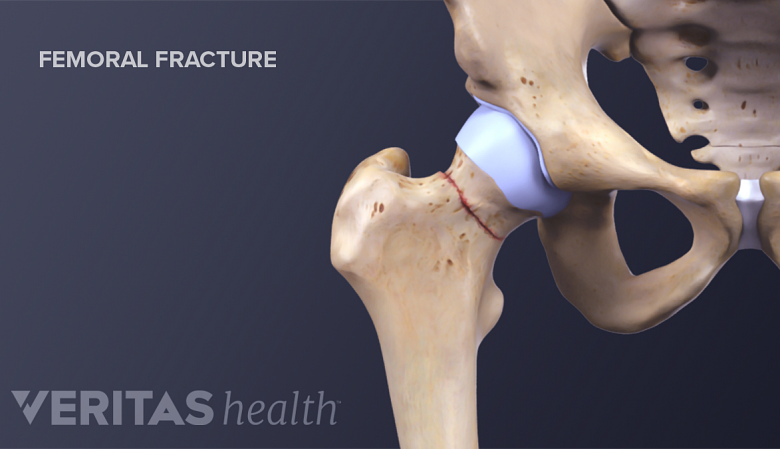
Although rare, complications such as a fracture of the femur near the hip can occur.
In This Article:
- Total Hip Replacement for Hip Arthritis
- Indications and Eligibility for Total Hip Replacement Surgery
- Total Hip Replacement Surgical Procedure
- Additional Facts and Considerations for Total Hip Replacement Surgery
- Total Hip Replacement Surgery Recovery
- Total Hip Replacement Surgery Risks and Complications
Complications Involving Anesthesia
Like any major surgery involving general anesthesia, hip replacement surgery carries a low risk of blood clots, stroke, heart attack, arrhythmia, and pneumonia.
Blood clots
One of the most common serious medical complications related to joint replacement surgery is blood clots.
- Deep vein thrombosis (DVT) refers to a blood clot in the leg and is called a deep vein thrombosis. A sudden increase in leg swelling along with calf tenderness may be the first sign of a blood clot in the leg.
- Pulmonary embolus (PE) refers to a clot that breaks off and travels to the lungs. Chest pain, an unusually fast heart rate or shortness of breath may indicate a pulmonary embolus.
Getting out of bed shortly after surgery (under doctor supervision) and following physical therapy guidelines will decrease the risk of blood clots. Patients are routinely prescribed medications after surgery to further minimize the risk of blood clots.
Patients experiencing symptoms of DVT or PE in the weeks to months following surgery should promptly call their surgeon or seek other medical attention.
Hip Dislocation
When the hip joint dislocates, the prosthetic ball comes out of its socket. It can usually be returned to its proper place without surgery, though this does require anesthesia and manipulation of the hip back into position.
Experts estimate 1% to 3% of people dislocate their new hips. 1 Brown ML, Ezzet KA. Relaxed Hip Precautions Do Not Increase Early Dislocation Rate Following Total Hip Arthroplasty. J Am Acad Orthop Surg. 2019 Sep 25;. doi: 10.5435/JAAOS-D-19-00261. [Epub ahead of print] PubMed PMID: 31567897. , 2 Ertaş ES, Tokgözoğlu AM. Dislocation after total hip arthroplasty: does head size really matter?. Hip Int. 2020 Jan 8;:1120700019898404. doi: 10.1177/1120700019898404. [Epub ahead of print] PubMed PMID: 31912749. , 3 Harkess, JW and Crockarell, JR Jr. Arthroplasty of the Hip. Campbell’s Operative Orthopedics, 13th edition. Philidelphia, PA. Elsevier, 2017: 167-321. For more than 40% of these people, hip dislocation is a one-time event. 4 Blom et al. Dislocation following total hip replacement: the Avon Orthopaedic Centre experience. Ann R Coll Surg Engl. 2008 Nov;90(8):658-62.
Dislocation is more likely in patients who:
- Are female
- Are older
- Have had a previous hip surgery (particularly a previous hip replacement)
- Have weak muscles surrounding the hip
- Had hip replacement surgery for a broken hip (femoral neck fracture)
- Have poor hip stability due to osteonecrosis, inflammatory arthritis (such as rheumatoid arthritis), or another pre-existing condition
Patients may be asked to avoid certain movements and activities that increase the likelihood of dislocation. For example, some patients who have had a posterior approach hip replacement may be advised not to sit in low seats or cross their legs in the weeks following surgery.
Infection
Some superficial wound infections can be treated with antibiotics; however, a deep infection often requires a minimum of one if not two additional surgical procedures.
- Experts estimate infection is diagnosed in 1% to 2% of hip replacement patients.
- The risk is highest for people who are overweight and/or have diabetes, anemia, inflammatory diseases such as rheumatoid arthritis, sickle cell disease, or blot clotting disorders.
- While the risk of infection decreases as the surgical wounds heal, it never completely goes away. People may be advised to take antibiotics ahead of invasive procedures to help prevent potential bacterial infections from spreading to the implant.
Viral infections, such as the flu, do not pose a risk to the hip implant.
See “When Can I…?” Answers for Hip Replacement Patients
Different Leg Lengths after Surgery
Orthopedic surgeons plan and operate very carefully to make sure the affected leg is the correct length. In some cases, the leg may be made slightly shorter or longer to optimize pain relief, joint stability, and joint mobility. 3 Harkess, JW and Crockarell, JR Jr. Arthroplasty of the Hip. Campbell’s Operative Orthopedics, 13th edition. Philidelphia, PA. Elsevier, 2017: 167-321. Small differences in leg length can be remedied with special shoe inserts.
Notably, the affected leg may initially feel longer, because the patient is used to standing and walking on an arthritic hip that has suffered a loss of joint space. In these cases, the patient just needs time to get used to the new hip.
Damage to Structures Around the Joint
It is possible for soft tissue (muscles, ligaments and tendons) around the hip to be damaged during the surgery. In rare cases there is damage to the surrounding arteries and veins (0.4%) and/or nerves (0.5%),3 which can result in leg weakness or decreased feeling in the leg.
Loosening of the Prosthetic
The new ball and socket should fit snuggly and securely with the existing natural bone. Over time, it is expected that the bones will heal to the surfaces of the porous metal implants. In rare cases this unfortunately may not occur. Over a longer time period, one or both prostheses may loosen their bond to bone. This loosening may (but will not always) cause pain and other problems, such as poor joint biomechanics, and necessitate further surgery.
The risk of prosthetic loosening increases over time. It is one of the reasons for needing a second (or revision) hip replacement.
Femur Fracture
The thighbone, or femur, can fracture during surgery, when the surgeon dislocates the hip’s ball and socket, or when the surgeon fits the prosthetic stem inside the femur. Fractures can also happen after surgery. About 2% of people experience a femur fracture after surgery.3 This complication often requires further surgery.
Death
Hip replacement is a major surgery and some complications, such as infection and blood clots, can be life-threatening.
Experts estimate 3 Harkess, JW and Crockarell, JR Jr. Arthroplasty of the Hip. Campbell’s Operative Orthopedics, 13th edition. Philidelphia, PA. Elsevier, 2017: 167-321. 0.35% (35 in 10,000) patients die within 30 days of hip replacement surgery. That rate changes to 1% (1 in 100) within 90 days of surgery. Men, people over age 70, and people who have heart disease or renal insufficiency are at greater risk of dying.
Considering Potential Complications
When thinking about potential complications, remember:
- The complications described here are not mutually exclusive—for example, a person may dislocate their new hip and fracture their femur at the same time.
- Not all of the complications described above will have long-term repercussions. For example, a blood clot or superficial wound infection may be treated successfully and have little to no long-term impact on the overall health of the patient or life of the new hip.
Patients are advised to ask their doctor about their unique individual risks for potential complications.
Most people do not experience serious complications and have less pain and better hip mobility after recovery.
- 1 Brown ML, Ezzet KA. Relaxed Hip Precautions Do Not Increase Early Dislocation Rate Following Total Hip Arthroplasty. J Am Acad Orthop Surg. 2019 Sep 25;. doi: 10.5435/JAAOS-D-19-00261. [Epub ahead of print] PubMed PMID: 31567897.
- 2 Ertaş ES, Tokgözoğlu AM. Dislocation after total hip arthroplasty: does head size really matter?. Hip Int. 2020 Jan 8;:1120700019898404. doi: 10.1177/1120700019898404. [Epub ahead of print] PubMed PMID: 31912749.
- 3 Harkess, JW and Crockarell, JR Jr. Arthroplasty of the Hip. Campbell’s Operative Orthopedics, 13th edition. Philidelphia, PA. Elsevier, 2017: 167-321.
- 4 Blom et al. Dislocation following total hip replacement: the Avon Orthopaedic Centre experience. Ann R Coll Surg Engl. 2008 Nov;90(8):658-62.