PRP has been used in surgeries to promote cell regeneration since 1987, 1 Ferrari M, Zia S, Valbonesi M. A new technique for hemodilution, preparation of autologous platelet-rich plasma and intraoperative blood salvage in cardiac surgery. Int J Artif Organs. 1987;10:47–50. , 2 Marx R, Garg A. Dental and craniofacial applications of platelet- rich plasma. Carol Stream: Quintessence Publishing Co, Inc.; 2005. and a growing body of evidence shows it is a viable treatment for tendinosis. 3 Kajikawa Y, Morihara T, Sakamoto H, Matsuda K, Oshima Y, Yoshida A, Nagae M, Arai Y, Kawata M, Kubo T. Platelet-rich plasma enhances the initial mobilization of circulation-derived cells for tendon healing. J Cell Physiol. 2008 Jun;215(3):837-45. doi: 10.1002/jcp.21368. PubMed PMID: 18181148. , 4 Sánchez M, Anitua E, Azofra J, Andía I, Padilla S, Mujika I. Comparison of surgically repaired Achilles tendon tears using platelet-rich fibrin matrices. Am J Sports Med. 2007 Feb;35(2):245-51. , 5 Mishra A, Pavelko T. Treatment of chronic elbow tendinosis with buffered platelet-rich plasma. Am J Sports Med. 2006 Nov;34(11):1774-8. Epub 2006 May 30. PubMed PMID: 16735582. , 6 Mishra AK, Skrepnik NV, Edwards SG, Jones GL, Sampson S, Vermillion DA, Ramsey ML, Karli DC, Rettig AC. Platelet-Rich Plasma Significantly Improves Clinical Outcomes in Patients With Chronic Tennis Elbow: A Double-Blind, Prospective, Multicenter, Controlled Trial of 230 Patients. Am J Sports Med. 2013 Jul 3. [Epub ahead of print] PubMed PMID: 23825183. Not until recently, though, have experts researched and debated whether or not platelet-rich plasma (PRP) injections are an effective treatment for osteoarthritis.
Recent studies on using PRP therapy to treat osteoarthritis have shown promising results.
In This Article:
- Platelet-Rich Plasma (PRP) Therapy for Arthritis
- PRP Injection Preparation and Composition
- Efficacy of Platelet-Rich Plasma Injections
- Potential Pros and Cons of PRP Injections
- Choosing a PRP Therapy Doctor
- Who Is a Candidate for Platelet-Rich Plasma Therapy?
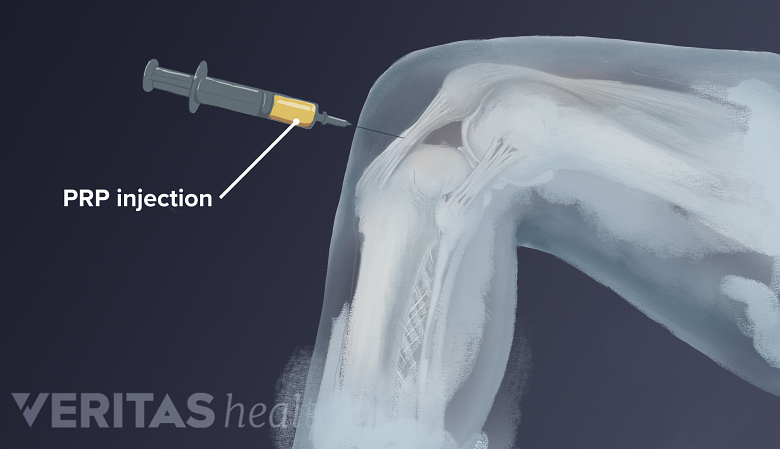
- Platelet-Rich Plasma Injection Procedure
Nearly all of the research investigating the use of PRP to treat osteoarthritis and other cartilage defects has been done since 2000, and the vast majority of research articles on the topic have been published since 2010.
Not all studies support the use of PRP to treat osteoarthritis; however, experts who have reviewed the existing body of research believe the evidence is largely encouraging and merits further investigation. 7 Smyth NA, Murawski CD, Fortier LA, Cole BJ, Kennedy JG. Platelet-rich plasma in the pathologic processes of cartilage: review of basic science evidence. Arthroscopy. 2013 Aug;29(8):1399-409. doi: 10.1016/j.arthro.2013.03.004. Epub 2013 May 11. PubMed PMID: 23669235. , 8 Kon E, Filardo G, Matteo BD, Marcacci M. PRP For the Treatment of Cartilage Pathology. Open Orthop J. 2013 May 3;7:120-8. doi: 10.2174/1874325001307010120. Print 2013. PubMed PMID: 23730375; PubMed Central PMCID: PMC3664439. , 9 Lee KS, Wilson JJ, Rabago DP, Baer GS, Jacobson JA, Borrero CG. Musculoskeletal applications of platelet-rich plasma: fad or future? AJR Am J Roentgenol. 2011 Mar;196(3):628-36. doi: 10.2214/AJR.10.5975. Review. PubMed PMID: 21343507.
Knee Osteoarthritis Treated with PRP
Researchers studying PRP and osteoarthritis often work with patients who have knee osteoarthritis, a condition that experts estimate will affect nearly half of all Americans at some point during their lives. 10 Center for Disease Control. Spotlight Osteoarthritis: Lifetime Risk of Symptomatic Knee Osteoarthritis. Updated October 20, 2010. www.cdc.gov. Accessed October 22, 2013. Two clinical studies that examine PRP to treat knee arthritis are described below.
- One study, published in 2013, involved 78 patients with osteoarthritis in both knees (156 knees).
11
Patel S, Dhillon MS, Aggarwal S, Marwaha N, Jain A. Treatment with platelet-rich plasma is more effective than placebo for knee osteoarthritis: a prospective, double-blind, randomized trial. Am J Sports Med. 2013 Feb;41(2):356-64. doi: 10.1177/0363546512471299. Epub 2013 Jan 8. PubMed PMID: 23299850.
Each knee received one of three treatments: 1 PRP injection, 2 PRP injections, or 1 placebo saline injection. Researchers evaluated the subjects' knees 6 weeks, 3 months, and 6 months after injection. Researchers found:
- Knees treated with 1 or 2 PRP injections saw a reduction in pain and stiffness as well as improvement in knee function at 6 weeks and 3 months.
- At the 6-month mark positive results declined, though pain and function were still better than before PRP treatment.
- The group that received placebo injections saw a small increase in pain and stiffness and a decrease in knee function.
The platelet-rich plasma used in this clinical study had 3 times the platelet concentration of normal blood and had been filtered to remove white blood cells.
- A second, smaller study examined patients who had experienced mild knee pain for an average of 14 months.
12
Halpern B, Chaudhury S, Rodeo SA, Hayter C, Bogner E, Potter HG, Nguyen J. Clinical and MRI outcomes after platelet-rich plasma treatment for knee osteoarthritis. Clin J Sport Med. 2013 May;23(3):238-9. doi: 10.1097/JSM.0b013e31827c3846. PubMed PMID: 23238250.
Each arthritic knee underwent an MRI to evaluate joint damage and then received a single PRP injection. Patients' knees were assessed at the 1 week, 3 month, 6 month and 1 year marks. In addition, each knee underwent a second MRI after one year. Researchers found:
- One year after receiving a PRP injection, most patients had less pain than they did the year before (though pain had not necessarily disappeared).
- MRIs showed that that the degenerative process had not progressed in the majority of knees.
While knee cartilage did not seem to regenerate for patients, the fact that the arthritis did not worsen may be significant. Evidence suggests that an average of 4 to 6% of cartilage disappears each year in arthritic joints. 13 Eckstein F, Cicuttini F, Raynauld JP, et al. Magnetic resonance imaging (MRI) of articular cartilage in knee osteoarthritis (OA): morphological assessment. Osteoarthr Cartilage. 2006;14:46–75. , 14 Raynauld JP, Martel-Pelletier J, Berthiaume MJ, et al. Long term eval- uation of disease progression through the quantitative magnetic reso- nance imaging of symptomatic knee osteoarthritis patients: correlation with clinical symptoms and radiographic changes. Arthitis Res Ther. 2006;8:21.
PRP Does Not Work for Everyone
Not all clinical studies provide evidence that PRP alleviates osteoarthritis symptoms. In several clinical studies PRP injections were no better than a placebo treatment. Even in studies that do provide evidence that PRP works, not all patients benefit.
See Is Stem Cell Therapy for Arthritis Safe and Effective?
PRP proponents assert that PRP fails to successfully treat symptoms in some cases because of differences in PRP formulation or injection administration - in other words, certain changes in variables, such as PRP preparation methods, the amount of PRP injected, and the frequency of injections, can make the PRP less effective. Others suggest that PRP therapy may be a passing fad that has limited value. 15 Lee KS, Wilson JJ, Rabago DP, Baer GS, Jacobson JA, Borrero CG. Musculoskeletal applications of platelet-rich plasma: fad or future? AJR Am J Roentgenol. 2011 Mar;196(3):628-36. doi: 10.2214/AJR.10.5975. Review. PubMed PMID: 21343507. , 16 Kolata G. As Sports Medicine Surges, Hope and Hype Outpace Proven Treatments. The New York Times. Sept 4 2011. www.nytimes.com. Accessed October 8, 2013.
It may be that PRP therapy, like other osteoarthritis treatments, works for some people but not for others, or works best in conjunction with other treatments, such as physical therapy.
Read more: Knee Exercises for Arthritis
- 1 Ferrari M, Zia S, Valbonesi M. A new technique for hemodilution, preparation of autologous platelet-rich plasma and intraoperative blood salvage in cardiac surgery. Int J Artif Organs. 1987;10:47–50.
- 2 Marx R, Garg A. Dental and craniofacial applications of platelet- rich plasma. Carol Stream: Quintessence Publishing Co, Inc.; 2005.
- 3 Kajikawa Y, Morihara T, Sakamoto H, Matsuda K, Oshima Y, Yoshida A, Nagae M, Arai Y, Kawata M, Kubo T. Platelet-rich plasma enhances the initial mobilization of circulation-derived cells for tendon healing. J Cell Physiol. 2008 Jun;215(3):837-45. doi: 10.1002/jcp.21368. PubMed PMID: 18181148.
- 4 Sánchez M, Anitua E, Azofra J, Andía I, Padilla S, Mujika I. Comparison of surgically repaired Achilles tendon tears using platelet-rich fibrin matrices. Am J Sports Med. 2007 Feb;35(2):245-51.
- 5 Mishra A, Pavelko T. Treatment of chronic elbow tendinosis with buffered platelet-rich plasma. Am J Sports Med. 2006 Nov;34(11):1774-8. Epub 2006 May 30. PubMed PMID: 16735582.
- 6 Mishra AK, Skrepnik NV, Edwards SG, Jones GL, Sampson S, Vermillion DA, Ramsey ML, Karli DC, Rettig AC. Platelet-Rich Plasma Significantly Improves Clinical Outcomes in Patients With Chronic Tennis Elbow: A Double-Blind, Prospective, Multicenter, Controlled Trial of 230 Patients. Am J Sports Med. 2013 Jul 3. [Epub ahead of print] PubMed PMID: 23825183.
- 7 Smyth NA, Murawski CD, Fortier LA, Cole BJ, Kennedy JG. Platelet-rich plasma in the pathologic processes of cartilage: review of basic science evidence. Arthroscopy. 2013 Aug;29(8):1399-409. doi: 10.1016/j.arthro.2013.03.004. Epub 2013 May 11. PubMed PMID: 23669235.
- 8 Kon E, Filardo G, Matteo BD, Marcacci M. PRP For the Treatment of Cartilage Pathology. Open Orthop J. 2013 May 3;7:120-8. doi: 10.2174/1874325001307010120. Print 2013. PubMed PMID: 23730375; PubMed Central PMCID: PMC3664439.
- 9 Lee KS, Wilson JJ, Rabago DP, Baer GS, Jacobson JA, Borrero CG. Musculoskeletal applications of platelet-rich plasma: fad or future? AJR Am J Roentgenol. 2011 Mar;196(3):628-36. doi: 10.2214/AJR.10.5975. Review. PubMed PMID: 21343507.
- 10 Center for Disease Control. Spotlight Osteoarthritis: Lifetime Risk of Symptomatic Knee Osteoarthritis. Updated October 20, 2010. www.cdc.gov. Accessed October 22, 2013.
- 11 Patel S, Dhillon MS, Aggarwal S, Marwaha N, Jain A. Treatment with platelet-rich plasma is more effective than placebo for knee osteoarthritis: a prospective, double-blind, randomized trial. Am J Sports Med. 2013 Feb;41(2):356-64. doi: 10.1177/0363546512471299. Epub 2013 Jan 8. PubMed PMID: 23299850.
- 12 Halpern B, Chaudhury S, Rodeo SA, Hayter C, Bogner E, Potter HG, Nguyen J. Clinical and MRI outcomes after platelet-rich plasma treatment for knee osteoarthritis. Clin J Sport Med. 2013 May;23(3):238-9. doi: 10.1097/JSM.0b013e31827c3846. PubMed PMID: 23238250.
- 13 Eckstein F, Cicuttini F, Raynauld JP, et al. Magnetic resonance imaging (MRI) of articular cartilage in knee osteoarthritis (OA): morphological assessment. Osteoarthr Cartilage. 2006;14:46–75.
- 14 Raynauld JP, Martel-Pelletier J, Berthiaume MJ, et al. Long term eval- uation of disease progression through the quantitative magnetic reso- nance imaging of symptomatic knee osteoarthritis patients: correlation with clinical symptoms and radiographic changes. Arthitis Res Ther. 2006;8:21.
- 15 Lee KS, Wilson JJ, Rabago DP, Baer GS, Jacobson JA, Borrero CG. Musculoskeletal applications of platelet-rich plasma: fad or future? AJR Am J Roentgenol. 2011 Mar;196(3):628-36. doi: 10.2214/AJR.10.5975. Review. PubMed PMID: 21343507.
- 16 Kolata G. As Sports Medicine Surges, Hope and Hype Outpace Proven Treatments. The New York Times. Sept 4 2011. www.nytimes.com. Accessed October 8, 2013.