There is no universally agreed-upon approach to post-surgical pain management. How to best relieve joint replacement patients’ pain is continually researched and debated. One group of experts 1 Horlocker TT. Pain management in total joint arthroplasty: a historical review. Orthopedics. 2010 Sep;33(9 Suppl):14-9. doi: 10.3928/01477447-20100722-65. Review. PubMed PMID: 20839717. suggests that most joint replacement patients should have a pain relief program that:
- Stops pain before it starts
- Limits exposure to painkillers called opioids (narcotics) by using multimodal analgesia
- May include peripheral nerve blocks
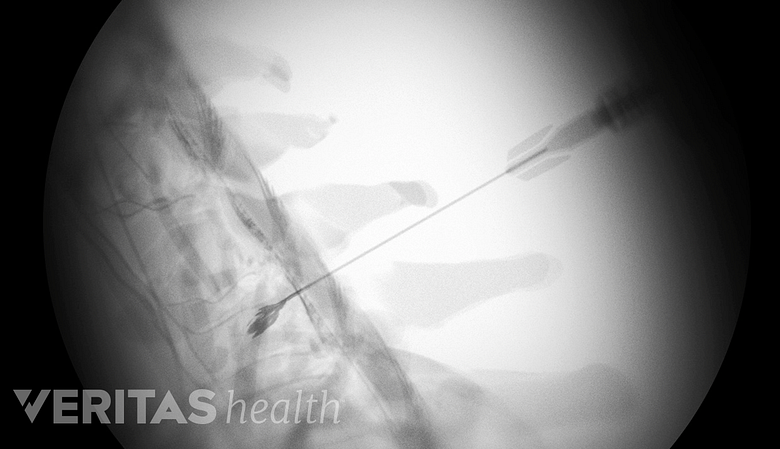
Nerve blockers can be injected to numb the sensation of nerves branching off from the spinal cord.
Each component of this program is described below. Also described are patient-controlled analgesic pumps.
In This Article:
- Managing the Pain of Joint Replacement
- What Pain Management Approach Works Best?
- Learn About Pain Management Before Surgery
Managing Pain Before It Starts
Patients can develop a heightened sensitivity to pain if it is left untreated. Neuropathways communicate pain sensations from the surgical site to the brain. Once that pathway is well worn, post-surgical pain can become more challenging to alleviate. Pre-emptive pain management helps patients avoid this scenario.
Pain medication may even be administered shortly before surgery. Following surgery, pain medications may be administered in regularly scheduled doses throughout the day.
See Pain Medications for Arthritis Pain Relief
Mulitmodal Analgesia
Doctors may use a combination of pain relief methods that complement each other and minimize side effects, an approach that is called multimodal analgesia.
Examples of multimodal analgesia
There is no single correct approach to multimodal analgesia. For example, joint replacement patients may receive:
- A peripheral nerve block (described below) and pain medications called non-steroidal anti-inflammatory drugs (NSAIDs)
- NSAIDs as well as steroids that decrease inflammation and pain
- An injection of local anesthetic into the bone around the joint during surgery in order to reduce post-surgical pain, in addition to NSAIDs and/or steroids
These pain-relieving strategies can augment or replace opioid medications, so that the patient requires fewer (or less potent) doses of narcotic medication.
Limiting the use of narcotic pain medications (opioids)
Medical professionals and patients rely on narcotics to quickly alleviate or lessen moderate to severe pain. While they are valuable and often necessary tools to manage pain, opioid painkillers should be used judiciously because:
- Opioids can leave some patients in a brain fog and feeling fatigued, nauseous, and/or constipated
- The side effects can make a patient feel unable or unwilling to participate in rehabilitation exercises
- Opioids can be addictive to certain people
Opioids are administered in different ways, including via pills, skin patches, injections, or intravenously. They are sold as prescription pills under brand names such as Percocet, OxyContin, and Vicodin.
In most cases, joint replacement patients benefit from a limited use of narcotic pain medication.
Peripheral Nerve Blocks
This anesthetic approach stops sensation at the nerve roots, where nerves branch off from the spinal cord. Only the specific limb on which the surgeon is operating is affected. For example, a patient undergoing shoulder replacement may receive a peripheral nerve block to the brachial plexus, a group of nerves that emerge through the cervical spine to enervate the shoulder and arm.
- A peripheral nerve block, sometimes called a peripheral anesthetic, is administered before surgery and lasts approximately 36 hours.
- It can be used in combination with a shorter-acting general anesthesia that puts the patient to sleep during surgery.
- When this approach is used, a patient can wake up from general anesthesia and have little to no pain in the affected limb.
Some experts recommend that joint replacement surgeries include the use of peripheral nerve blocks, and many clinical studies support their use, citing their ability to control pain and facilitate recovery. 2 Hebl JR, Dilger JA, Byer DE, Kopp SL, Stevens SR, Pagnano MW, Hanssen AD, Horlocker TT. A pre-emptive multimodal pathway featuring peripheral nerve block improves perioperative outcomes after major orthopedic surgery. Reg Anesth Pain Med. 2008 Nov-Dec;33(6):510-7. PubMed PMID: 19258965. , 3 Macfarlane AJR, Arun Prasad G, Chan VWS, Brull R. Does Regional Anesthesia Improve Outcome After Total Knee Arthroplasty? Clinical Orthopaedics and Related Research 2009;467(9):2379-2402. doi:10.1007/s11999-008-0666-9.
Not all surgeons use peripheral nerve blocks. Reason for this include:
- They may interfere with patients’ ability to participate in physical therapy shortly after surgery.
- Some research suggests that peripheral nerve blocks may contribute to hip and knee replacement patients falling during the early recovery period, 4 Pelt CE, Anderson AW, Anderson MB, Van Dine C, Peters CL. Postoperative falls after total knee arthroplasty in patients with a femoral nerve catheter: can we reduce the incidence? J Arthroplasty. 2014 Jun;29(6):1154-7. doi: 10.1016/j.arth.2014.01.006. Epub 2014 Jan 16. PubMed PMID: 24581899. , 5 Sharma S, Iorio R, Specht LM, Davies-Lepie S, Healy WL. Complications of femoral nerve block for total knee arthroplasty. Clin Orthop Relat Res. 2010 Jan;468(1):135-40. doi: 10.1007/s11999-009-1025-1. Epub 2009 Aug 13. PubMed PMID: 19680735; PubMed Central PMCID: PMC2795813. and therefore should be avoided or used with caution.
Whether a surgeon uses peripheral nerve block will depend upon many factors, including the surgeon’s preference, the hospital’s pain management policy, and the patient’s circumstances.
Patient-Controlled Intravenous Analgesia
While it's not a part of the pain management strategy described above, many doctors and hospitals give patients control of their own pain medication. For example, during their post-operative hospital stay, joint replacement patients may be given a patient-controlled analgesia (PCA) pump.
See Anesthesia for Orthopedic Surgery
With a PCA pump, a patient can press a button to self-administer doses of pain-relieving drugs through an existing IV line. PCA pumps typically deliver opioid medications, such as morphine or fentanyl. A pump is programmed to deliver doses specific to the patient, so there is no risk of overdose.
Many doctors like this method of treatment because it gives patients a sense of control over their pain. Some doctors prefer not to rely on it because patients may not control pain adequately or consistently.
- 1 Horlocker TT. Pain management in total joint arthroplasty: a historical review. Orthopedics. 2010 Sep;33(9 Suppl):14-9. doi: 10.3928/01477447-20100722-65. Review. PubMed PMID: 20839717.
- 2 Hebl JR, Dilger JA, Byer DE, Kopp SL, Stevens SR, Pagnano MW, Hanssen AD, Horlocker TT. A pre-emptive multimodal pathway featuring peripheral nerve block improves perioperative outcomes after major orthopedic surgery. Reg Anesth Pain Med. 2008 Nov-Dec;33(6):510-7. PubMed PMID: 19258965.
- 3 Macfarlane AJR, Arun Prasad G, Chan VWS, Brull R. Does Regional Anesthesia Improve Outcome After Total Knee Arthroplasty? Clinical Orthopaedics and Related Research 2009;467(9):2379-2402. doi:10.1007/s11999-008-0666-9.
- 4 Pelt CE, Anderson AW, Anderson MB, Van Dine C, Peters CL. Postoperative falls after total knee arthroplasty in patients with a femoral nerve catheter: can we reduce the incidence? J Arthroplasty. 2014 Jun;29(6):1154-7. doi: 10.1016/j.arth.2014.01.006. Epub 2014 Jan 16. PubMed PMID: 24581899.
- 5 Sharma S, Iorio R, Specht LM, Davies-Lepie S, Healy WL. Complications of femoral nerve block for total knee arthroplasty. Clin Orthop Relat Res. 2010 Jan;468(1):135-40. doi: 10.1007/s11999-009-1025-1. Epub 2009 Aug 13. PubMed PMID: 19680735; PubMed Central PMCID: PMC2795813.