There are many reasons why knee bursitis may develop. When the underlying cause is identified, it can help guide choices for treatment as well as recommendations for preventing future bursitis flare-ups.
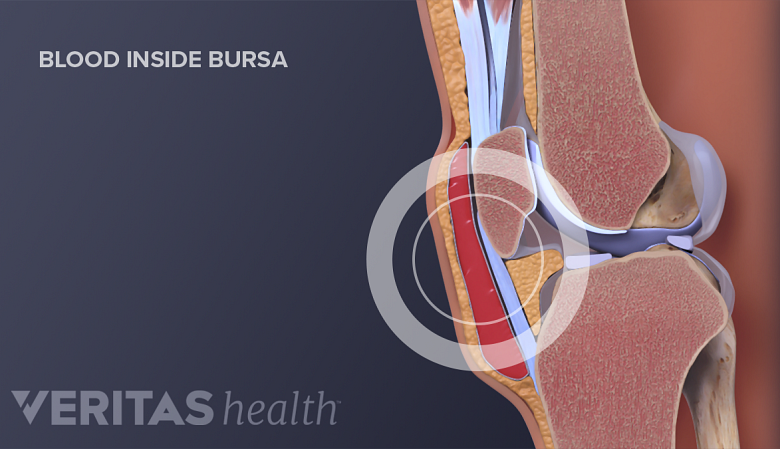
An injury to the knee could cause the prepatellar bursa to fill with blood and become inflamed.
This page describes several possible factors that cause or increase the risk of developing knee bursitis.
In This Article:
- Knee (Prepatellar) Bursitis
- Prepatellar Bursitis Symptoms
- Causes of Knee Bursitis (Prepatellar Bursitis)
- Prepatellar Bursitis Diagnosis
- Prepatellar Bursitis Treatment
- Pes Anserine Bursitis Video
Causes and Risk Factors for Knee Bursitis
While repetitive irritation, trauma, or infection may trigger knee bursitis, the underlying cause cannot always be identified. Certain factors, such as underlying conditions, can increase the risk of knee bursitis.
Repetitive irritation to the bursa
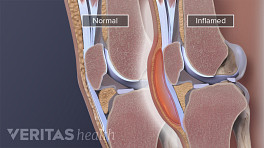
Knee bursitis is often caused by frequent mini-traumas, such as repetitive kneeling on hard surfaces. Kneeling puts pressure on the front of the knee, where the prepatellar bursa is located.
- Mini-traumas can irritate the bursa’s delicate lining, leading to inflammation.
- The inflammation may cause the bursal lining to produce excess synovial fluid.
- The excess fluid builds up in the bursa sac, causing it to swell and leading to knee bursitis symptoms.
People who kneel a lot for their work, such as carpet installers, roofers, housecleaners, and clergy, may develop bursitis in their knees. Intense exercise, such as jogging or power-lifting, may also be associated with knee bursitis. 1 Parker CH, Leggit JC. Novel Treatment of Prepatellar Bursitis. Mil Med. 2018 Nov 1;183(11-12):e768-e770. doi: 10.1093/milmed/usy098. PMID: 29800302.
Trauma to the knee
An acute injury can damage the prepatellar bursa at the front of the knee. When this happens, the bursa may become swollen with blood, synovial fluid, or a combination of the two. After an injury:
- The damaged prepatellar bursa may fill with blood.
- The blood irritates the bursa’s delicate lining, causing it to become inflamed.
- While the blood in the prepatellar bursa may be gradually reabsorbed into the body, the bursa’s lining may stay inflamed. The inflamed lining may produce excess synovial fluid.
- The fluid fills the bursa, causing swelling and other knee bursitis symptoms.
If a doctor uses a needle and syringe to draw fluid from a bursa after a trauma, the fluid may appear reddish or pink because of the presence of blood.
Another underlying condition
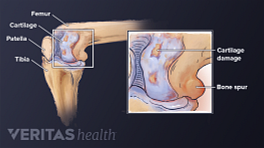
While not common, a prepatellar bursa can become inflamed as the result of another condition, such as rheumatoid arthritis or gout. 2 Rishor-Olney CR, Pozun A. Prepatellar Bursitis. 2020 May 30. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan–. PMID: 32491440. In these instances, the treatment for knee bursitis must accompany treatment for the underlying condition.
Infection (septic bursitis)
Knee bursitis can be caused by an infection, a condition called septic bursitis. Certain medical conditions, such as diabetes, alcoholism, and rheumatoid arthritis, increase the risk of developing septic bursitis. 3 Lormeau C, Cormier G, Sigaux J, Arvieux C, Semerano L. Management of septic bursitis. Joint Bone Spine. 2019 Oct;86(5):583-588. doi: 10.1016/j.jbspin.2018.10.006. Epub 2018 Oct 26. PMID: 31615686. , 4 Khodaee M. Common Superficial Bursitis. Am Fam Physician. 2017 Feb 15;95(4):224-231. PMID: 28290630. Risk may also be increased by certain medications that suppress the immune system.
Children are also susceptible to septic prepatellar bursitis. 2 Rishor-Olney CR, Pozun A. Prepatellar Bursitis. 2020 May 30. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan–. PMID: 32491440.
History of inflammation of the prepatellar bursa
People who have had bursitis in the past have an increased chance of developing bursitis again. For this reason, people who have had prepatellar bursitis are encouraged to take steps to prevent future flare-ups. For example, a carpet installer who kneels a lot for work can wear knee pads.
By addressing these causes and risk factors, an individual can decrease the likelihood of developing chronic knee bursitis.
- 1 Parker CH, Leggit JC. Novel Treatment of Prepatellar Bursitis. Mil Med. 2018 Nov 1;183(11-12):e768-e770. doi: 10.1093/milmed/usy098. PMID: 29800302.
- 2 Rishor-Olney CR, Pozun A. Prepatellar Bursitis. 2020 May 30. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan–. PMID: 32491440.
- 3 Lormeau C, Cormier G, Sigaux J, Arvieux C, Semerano L. Management of septic bursitis. Joint Bone Spine. 2019 Oct;86(5):583-588. doi: 10.1016/j.jbspin.2018.10.006. Epub 2018 Oct 26. PMID: 31615686.
- 4 Khodaee M. Common Superficial Bursitis. Am Fam Physician. 2017 Feb 15;95(4):224-231. PMID: 28290630.