Significant, site-specific swelling can make elbow bursitis easy to identify. Nonetheless, a doctor must rule out other possible elbow problems, such as arthritis, tendinitis, a fracture, and sarcoma (tumor), 1 Blackwell JR, Hay BA, Bolt AM, Hay SM. Olecranon bursitis: a systematic overview. Shoulder Elbow 2014;6:182-90. http://dx.doi.org/10.1177/1758573214532787 before making a diagnosis of elbow bursitis. To do this, a doctor will use a combination of diagnostic tools.
For elbow bursitis to be diagnosed, other conditions must first be ruled out.
In This Article:
- Elbow (Olecranon) Bursitis
- Elbow (Olecranon) Bursitis Symptoms
- Elbow (Olecranon) Bursitis Causes
- Elbow (Olecranon) Bursitis Diagnosis
- Elbow (Olecranon) Bursitis Treatment
Medical Visit
A physician or other licensed medical care provider can conduct a:
- Patient interview. The doctor will ask a patient to describe the onset of symptoms and the pattern of pain and swelling. In addition, information about the patient’s medical history, occupation, and hobbies can provide important clues as to whether the elbow’s bursa is infected (septic bursitis). 1 Blackwell JR, Hay BA, Bolt AM, Hay SM. Olecranon bursitis: a systematic overview. Shoulder Elbow 2014;6:182-90. http://dx.doi.org/10.1177/1758573214532787
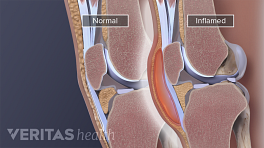
- Physical exam. The doctor will examine the patient’s joint, noting swelling at the elbow, tenderness and pain points, and range of motion.
Inflammation of the elbow bursa is usually visible and palpable, so the physical exam is an important part of the diagnosis.
Testing skin temperature
One way to possibly determine if the bursa is infected is to compare the skin temperature of the affected elbow to that of the unaffected elbow. In one study,
2
Smith DL, McAfee JH, Lucas LM, Kumar KL, Romney DM, "Septic and nonseptic olecranon bursitis. Utility of the surface temperature probe in the early differentiation of septic and nonseptic cases," (Abstract only) Arch Intern Med, 1989;149(7):1581-1585. PMID 2742432.
11 patients with septic elbow bursitis had skin temperature at least 2.2° C warmer (about 4° F warmer) on their affected elbows. In the same study, only 2 out of 35 patients with aseptic (non-infectious) elbow bursitis showed such a large temperature differential at their elbows' skin surfaces.
Other signs of possible infection include fever, elbow swelling that is acutely painful or tender, and redness of the skin over the elbow.
A doctor may also order medical imaging and/or lab tests. Because prompt treatment with antibiotics is recommended for septic arthritis, a doctor who strongly suspects septic bursitis in the elbow may prescribe antibiotics without definitive diagnostic testing.
Aspiration and Lab Tests
A doctor may perform an aspiration, removing fluid from the elbow’s bursa with a needle and syringe. In addition to relieving pressure and making the patient more comfortable, aspiration provides a fluid sample that can be tested for infection.
See What Is Arthrocentesis (Joint Aspiration)? and Diagnosis through Synovial Fluid Analysis
Additional lab testing.
Blood tests may also be used to help rule out or confirm systemic (body-wide) infection and inflammatory conditions, such as rheumatoid arthritis, psoriatic arthritis, and gout. These conditions can cause joint pain and increase the likelihood of developing bursitis, including elbow bursitis.
Medical Imaging
If it is unclear whether symptoms are caused by elbow bursitis or another condition, a doctor may request an:
- X-ray, which can show broken bones and signs of elbow osteoarthritis
- Magnetic resonance imaging (MRI), which can show detailed images of bone tissue as well as soft tissues near the elbow joint, including the triceps tendon. MRI can help rule out septic bursitis in some cases, but it cannot definitively distinguish between all cases of septic bursitis or aseptic bursitis. 3 Floemer F, Morrison WB, Bongartz G, Lederman HP, "MRI Characteristics of Olecranon Bursitis," American Journal of Roentgenology, 2004;183(1) 29-34.
- Ultrasound, which can detect areas of fluid, such as the excess synovial fluid found in a swollen bursa.
Medical imaging is not required for and accurate diagnosis in many cases.
Elbow bursitis is a likely cause of local swelling at the elbow. Most other medical conditions that can cause swelling at the elbow are musculoskeletal conditions that result from a trauma or repeated stress on the joint. The exception is sarcoma, a rare type of cancer. If swelling in the elbow does not respond to elbow bursitis treatment or is accompanied by unexplained weight loss then additional diagnostic testing for sarcoma may be recommended. 4 Blackwell JR, Hay BA, Bolt AM, Hay SM. Olecranon bursitis: a systematic overview. Shoulder Elbow 2014;6:182-90. http://dx.doi. org/10.1177/1758573214532787. As cited in Reilly D, Kamineni S. Olecranon bursitis. J Shoulder Elbow Surg. 2016 Jan;25(1):158-67. doi: 10.1016/j.jse.2015.08.032. Epub 2015 Nov 11. Review. PubMed PMID: 26577126.
Once a diagnosis of elbow bursitis has been made, treatment may begin.
- 1 Blackwell JR, Hay BA, Bolt AM, Hay SM. Olecranon bursitis: a systematic overview. Shoulder Elbow 2014;6:182-90. http://dx.doi.org/10.1177/1758573214532787
- 2 Smith DL, McAfee JH, Lucas LM, Kumar KL, Romney DM, "Septic and nonseptic olecranon bursitis. Utility of the surface temperature probe in the early differentiation of septic and nonseptic cases," (Abstract only) Arch Intern Med, 1989;149(7):1581-1585. PMID 2742432.
- 3 Floemer F, Morrison WB, Bongartz G, Lederman HP, "MRI Characteristics of Olecranon Bursitis," American Journal of Roentgenology, 2004;183(1) 29-34.
- 4 Blackwell JR, Hay BA, Bolt AM, Hay SM. Olecranon bursitis: a systematic overview. Shoulder Elbow 2014;6:182-90. http://dx.doi. org/10.1177/1758573214532787. As cited in Reilly D, Kamineni S. Olecranon bursitis. J Shoulder Elbow Surg. 2016 Jan;25(1):158-67. doi: 10.1016/j.jse.2015.08.032. Epub 2015 Nov 11. Review. PubMed PMID: 26577126.