When does a swollen knee require medical care, and when can it be treated at home? Mild to moderate knee swelling and knee effusion—sometimes called water on the knee—can usually be treated at home. Medical attention is recommended if the knee is persistently swollen or accompanied by severe pain or other serious symptoms.
Read on to learn when to contact a doctor, how to treat a swollen knee at home, and how doctors can remove fluid from a knee using a process called aspiration.
When to Contact a Doctor
Below are guidelines to help people decide if their knee swelling requires medical attention. If the person is still unsure whether to seek professional medical treatment, a phone call to a doctor or nurse can help determine whether an office visit is necessary.
A doctor should be contacted if:
- The knee is severely swollen or has a pronounced abnormality
- The knee cannot fully straighten or fully bend
- The knee is severely painful (for example, the pain is not adequately treated with over-the-counter medication)
- The person cannot bear weight on the knee, or feels as if the knee is going to "give out"
- The skin over the knee turns hot or red
- The person has a fever of 100.4° F or higher
- Knee swelling has been present for 3 days or longer
A doctor will examine the patient's knee and ask the patient several questions. The physical examination and patient interview may provide enough information to make an accurate diagnosis. If more information is needed, the doctor may recommend medical imaging, such as an x-ray, or removing fluid from the knee using an in-office procedure called aspiration. (Aspiration is described at the bottom of this page.)
Read about Arthritis Treatment Specialists
Leg swelling may be a cause for concern
Contact a doctor if the swelling affects the leg, not just the knee. Leg swelling can be a sign of a serious health problem.
1
Schellong SM, Wollina U, Unger L, Machetanz J, Stelzner C. Das geschwollene Bein [Leg swelling]. Internist (Berl). 2013;54(11):1294-1303. doi:10.1007/s00108-013-3339-z
,
2
Gorman WP, Davis KR, Donnelly R. ABC of arterial and venous disease. Swollen lower limb-1: general assessment and deep vein thrombosis [published correction appears in BMJ 2000 Jul 29;321(7256):266]. BMJ. 2000;320(7247):1453-1456. doi:10.1136/bmj.320.7247.1453
Seek immediate care if the leg swelling occurs suddenly with no known reason, particularly if it is accompanied by symptoms such as leg pain, chest pain, and/or problems breathing, as these may be signs of a life-threatening blood clot.
How to Treat a Swollen Knee at Home
In many cases, a mild to moderately swollen knee may be treated at home. Home care typically involves Rest, Ice, Compression, and Elevation (R.I.C.E.) and medication. Read the descriptions of these treatments below to help maximize their benefit and avoid mistakes.
The 4-step R.I.C.E. Formula
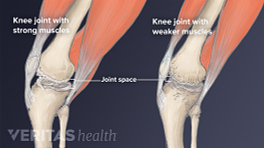
1. Rest will give the joint time to repair and recover. Take a break from sports and other activities for 24 hours or longer. The joint should not necessarily be immobile; people with knee swelling should try to gently flex and straighten the knee several times a day to maintain range of motion.
2. Icing is an easy, effective treatment for excess knee swelling. Cold therapy can ease symptoms by:
- Causing nearby blood vessels to constrict, decreasing blood flow and inflammation
- Slowing down the production of joint fluid in the knee (—synovial joint fluid is normally helpful but can contribute to knee swelling and discomfort)
- Distracting the brain from pain signals to the brain
Apply a cold compress to the knee for no longer than 20 minutes at a time. This can be done several times a day.
Ice should not be applied directly to the skin. Prevent skin damage by placing a towel or another material in between the icepack and skin. Cold therapy may not be appropriate for people who have Raynaud’s Syndrome or nerve damage.
See When and Why to Apply Cold to an Arthritic Joint
3. Compression involves wrapping the affected joint in an elastic bandage (such as an Ace bandage). Compression may help limit or reduce swelling.
A 3- to 4-inch wide bandage is typically recommended. (A smaller width bandage can increase the risk of cutting off circulation.) Loosen or re-wrap the bandage if it is too tight. Wrapping the swollen knee too tightly may cause increased swelling as well as numbness, tingling, increased pain, coolness, or swelling.
Keep in mind that a compression bandage will not support the knee or protect it from further injury.
4. Elevation
Elevating the affected leg can help reduce blood flow to the knee, helping to alleviate inflammation, swelling, and discomfort. Ideally, the affected leg should be elevated above the heart. To do this, lie down with the knee and calf propped up on pillows. Sitting down with the affected leg elevated on a stool or ottoman is considered less effective because the knee is below the heart.
People who cope with chronic knee swelling might consider purchasing a leg elevation pillow. These pillows are typically made out of foam and specially designed to provide firm, comfortable support.
Using the R.I.C.E. formula, swelling often goes down in 1 to 3 days. If the swelling does not go down within a few days of starting R.I.C.E., or if swelling and pain worsen, contact a doctor.
Read more about The P.R.I.C.E. Protocol Principles on Sports-health.com
Over-the-counter medication
While not always necessary, over-the-counter medication may be used to relieve knee swelling and associated pain.
Commonly recommended options include:
- Non-steroidal anti-inflammatory drugs, or NSAIDs, including ibuprofen and naproxen, which may reduce both pain and swelling
- Acetaminophen (Tylenol), which will not relieve swelling but may relieve associated pain
- Topical salicylates medications, sold under brand names such as Aspercreme and Sportscreme, which are applied directly to the skin over the affected knee and may reduce pain and swelling
Topical salicylates medications deliver a small dose of anti-inflammatory medication that is chemically similar to aspirin. These medications are typically recommended for arthritis joint pain. Do not use topical medications on cut or cracked skin or skin that has an infection or rash.
Joint or Bursal Aspiration
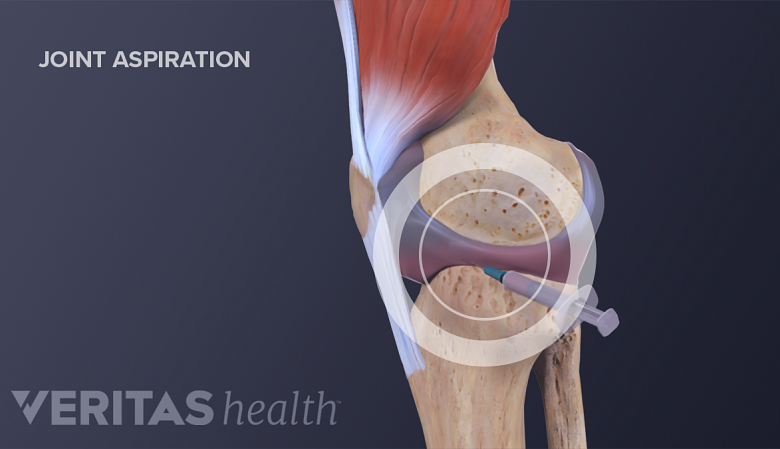
Joint aspiration is the process of removing fluid from the joint with a needle.
When a patient has a swollen knee, a doctor may want to verify or rule out certain diagnoses by analyzing the accumulated fluid. To do this, the doctor will remove fluid from the affected knee joint capsule or bursa using a needle and syringe. When performed on a joint capsule, this process is called joint aspiration or arthrocentesis. When performed on a bursa, this process is called bursal aspiration.
See What Is Arthrocentesis (Joint Aspiration)?
The doctor will take note of the aspirated fluid's color and viscosity and may send it to a lab for further analysis. Determining the contents of the fluid can lead to an accurate diagnosis. For example, uric acid crystals in the joint fluid indicate gout, and bacteria in the fluid indicate infection.
See The Joint Aspiration Procedure
Aspiration and examination of the fluid are important diagnostic steps because the underlying cause of knee swelling will determine the appropriate medical treatment.
Aspirated fluids are not always sent to a lab for analysis. If a diagnosis is already known, a physician may perform an aspiration to improve joint function and patient comfort.
- 1 Schellong SM, Wollina U, Unger L, Machetanz J, Stelzner C. Das geschwollene Bein [Leg swelling]. Internist (Berl). 2013;54(11):1294-1303. doi:10.1007/s00108-013-3339-z
- 2 Gorman WP, Davis KR, Donnelly R. ABC of arterial and venous disease. Swollen lower limb-1: general assessment and deep vein thrombosis [published correction appears in BMJ 2000 Jul 29;321(7256):266]. BMJ. 2000;320(7247):1453-1456. doi:10.1136/bmj.320.7247.1453