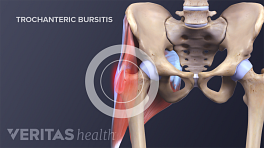
Hip osteoarthritis can be slightly challenging to diagnose because hip pain can be more diffuse, radiating to the low back and thigh, and mimic other conditions. Other conditions that may mimic hip arthritis include hip bursitis, tendonitis and muscle injuries, and bone fractures. Hip pain may also be referred pain caused by problems in nearby body parts, such as the sacroiliac joint or low back. A physician will use diagnostic tools to rule out other possible causes.
In This Article:
Patient interview
During an appointment a physician will ask the patient to describe the symptoms, including when the symptoms began; the pattern of pain and stiffness; and how symptoms affect his or her lifestyle. A patient’s reported symptoms are important for diagnosis and treatment.
Physical exam
A physician will test the hip’s range of motion and examine it for swelling and pain points. He or she will test muscles for weakness, because muscles play an important role in protecting the hip joint from osteoarthritis. The physician may also assess a person’s stride and other movements.
The physician may learn enough during the patient interview and physical exam to make an accurate diagnosis. If not, he or she may order medical imaging or lab tests. These diagnostic tools provide additional information that can reveal the extent of the hip arthritis and/or rule out other possible causes of the patient’s pain.
X-rays
Hip osteoarthritis can be confirmed with x-rays. X-rays show:
- How much space there is between the femur and the acetabulum of the pelvic bone (the hip’s ball and socket). No space or an abnormally small space indicates a loss of cartilage.
- Small bumps on the bones, called bone spurs or osteophytes. Bone spurs are a normal sign of aging—almost everyone over age 50 has some—but they may proliferate as bones try to compensate for cartilage loss. These growths can create additional friction that can lead to pain.
X-rays may show significant signs of hip osteoarthritis and yet the patient may not be in pain. Conversely, x-rays may show only mild osteoarthritis but the patient reports significant pain. Therefore, x-rays are just one tool to be used with the patient interview and physical exam.
MRI
Magnetic Resonance Imaging (MRI) can provide images of the hip’s soft tissues (such as the hip labrum, articular cartilage, and tendons) as well as bone. A doctor may order an MRI if the x-rays are inconclusive or he or she suspects something other than osteoarthritis, such as damage to the hip’s labrum. An MRI is not needed in most cases. MRIs tend to be more time-consuming and more expensive than x-rays.
Ultrasound
Ultrasound can be useful for evaluating the soft tissue structures that surround the hip joint, such as tendons, bursae, muscles, and the edge of the labrum. Ultrasound can also be used to identify changes to the delicate membrane that surrounds the joint (synovial lining) or an abnormal increase in joint fluid (synovial fluid). A physician may use ultrasound along with an injection of local anesthetic (intraarticular injection) to try to identify the exact source of pain.
Lab tests for other conditions
A doctor may order lab tests to diagnose or rule out other potential problems, such as infection or types of inflammatory arthritis, which can also cause hip pain. Lab tests may require a blood draw or an aspiration of the hip joint, during which fluid is taken from the hip.
See What Is Arthrocentesis (Joint Aspiration)?
In the future, doctors may be able to test blood or joint fluid for biomarkers that predict or identify the osteoarthritis. 1 Kraus VB, Collins JE, Hargrove D, Losina E, Nevitt M, Katz JN, Wang SX, Sandell LJ, Hoffmann SC, Hunter DJ; OA Biomarkers Consortium.. Predictive validity of biochemical biomarkers in knee osteoarthritis: data from the FNIH OA Biomarkers Consortium. Ann Rheum Dis. 2017 Jan;76(1):186-195. doi: 10.1136/annrheumdis-2016-209252. Epub 2016 Jun 13. PubMed PMID: 27296323; PubMed Central PMCID: PMC5851287. , 2 Van Spil WE, Nair SC, Kinds MB, Emans PJ, Hilberdink WK, Welsing PM, Lafeber FP. Systemic biochemical markers of joint metabolism and inflammation in relation to radiographic parameters and pain of the knee: data from CHECK, a cohort of early-osteoarthritis subjects. Osteoarthritis Cartilage. 2015 Jan;23(1):48-56. doi: 10.1016/j.joca.2014.09.003. Epub 2014 Sep 6. PubMed PMID: 25205017.
- 1 Kraus VB, Collins JE, Hargrove D, Losina E, Nevitt M, Katz JN, Wang SX, Sandell LJ, Hoffmann SC, Hunter DJ; OA Biomarkers Consortium.. Predictive validity of biochemical biomarkers in knee osteoarthritis: data from the FNIH OA Biomarkers Consortium. Ann Rheum Dis. 2017 Jan;76(1):186-195. doi: 10.1136/annrheumdis-2016-209252. Epub 2016 Jun 13. PubMed PMID: 27296323; PubMed Central PMCID: PMC5851287.
- 2 Van Spil WE, Nair SC, Kinds MB, Emans PJ, Hilberdink WK, Welsing PM, Lafeber FP. Systemic biochemical markers of joint metabolism and inflammation in relation to radiographic parameters and pain of the knee: data from CHECK, a cohort of early-osteoarthritis subjects. Osteoarthritis Cartilage. 2015 Jan;23(1):48-56. doi: 10.1016/j.joca.2014.09.003. Epub 2014 Sep 6. PubMed PMID: 25205017.