Before diagnosing osteoarthritis, a doctor must rule out other possible causes of joint pain, such as bursitis or rheumatoid arthritis. The diagnostic process involves taking the patient’s medical history and a physical examination, including evaluations of joint function and flexibility. Medical imaging, such as x-rays, and lab tests may also be ordered.
While a primary care physician can diagnose osteoarthritis, a person with joint pain may be referred to a specialist, such as a physiatrist, sports medicine physician, or orthopedic surgeon, for further evaluation.
This page provides details regarding the steps used to diagnose osteoarthritis.
In This Article:
- What Is Osteoarthritis?
- Osteoarthritis Symptoms and Signs
- Osteoarthritis Causes
- Osteoarthritis Diagnosis
- Osteoarthritis Treatment
Medical History
A physician will ask about the joint pain, including when it began, its severity, what activities make it better or worse, and if other symptoms are present. They may also ask about family history and day-to-day living. Thorough questioning and honest answers are important to making an accurate diagnosis and may also influence treatment choices.
Physical Examination
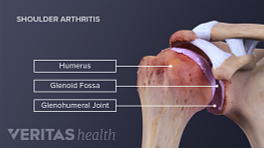
The physician will look for physical signs of arthritis, such as swelling, tenderness, and bone spurs that are visible under the skin. Physical tests will be used to assess the joint’s range of motion, strength, and function, as well as neurological health.
Medical Imaging
Medical imaging provides views of inside the body. Two types of medical imaging commonly used to diagnose osteoarthritis are x-rays and magnetic resonance imaging (MRI):
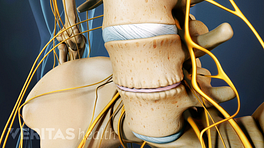
- X-rays can show how much space is between a joint’s bones, indicating whether there has been a loss of cartilage. An x-ray can also show bone spurs, a sign that the bones have tried to compensate for cartilage loss with extra bone growth.
- MRIs provide a detailed look at soft tissues, such as cartilage, ligaments, tendons, and muscle, as well as bone. While not required for an osteoarthritis diagnosis, an MRI may be ordered if to assess the joint’s soft tissues and/or rule out other possible diagnoses. MRIs take longer and are more expensive than x-rays.
- Ultrasound can be useful for evaluating the soft tissue structures that surround the affected joint, such as tendons. Ultrasound can also be used to identify changes to the delicate membrane that encapsulates the joint (synovial lining) or an abnormal increase in joint fluid (synovial fluid).
A physician may use ultrasound along with an injection of local anesthetic (intraarticular injection) to try to identify the exact source of pain.
Many individuals have signs of osteoarthritis that can be seen on medical imaging, even if they do not experience symptoms. Medical imaging is just one diagnostic tool and must be used in conjunction with the patient interview and physical exam.
Lab Tests
Currently, there is no standard lab test to verify the presence of osteoarthritis. Lab tests may be used to rule out other problems, such as rheumatoid arthritis, which also causes joint pain. Lab tests may require drawing fluid from the joint (arthrocentesis) or taking a blood sample.
In the future, labs may be able to test blood or joint fluid for biomarkers that predict or identify osteoarthritis. 1 Kraus VB, Collins JE, Hargrove D, Losina E, Nevitt M, Katz JN, Wang SX, Sandell LJ, Hoffmann SC, Hunter DJ; OA Biomarkers Consortium.. Predictive validity of biochemical biomarkers in knee osteoarthritis: data from the FNIH OA Biomarkers Consortium. Ann Rheum Dis. 2017 Jan;76(1):186-195. doi: 10.1136/annrheumdis-2016-209252. Epub 2016 Jun 13. PubMed PMID: 27296323; PubMed Central PMCID: PMC5851287. , 2 Van Spil WE, Nair SC, Kinds MB, Emans PJ, Hilberdink WK, Welsing PM, Lafeber FP. Systemic biochemical markers of joint metabolism and inflammation in relation to radiographic parameters and pain of the knee: data from CHECK, a cohort of early-osteoarthritis subjects. Osteoarthritis Cartilage. 2015 Jan;23(1):48-56. doi: 10.1016/j.joca.2014.09.003. Epub 2014 Sep 6. PubMed PMID: 25205017.
The above combination of medical history, physical exam, and possibly diagnostic testing, all inform the diagnosis of osteoarthritis.
- 1 Kraus VB, Collins JE, Hargrove D, Losina E, Nevitt M, Katz JN, Wang SX, Sandell LJ, Hoffmann SC, Hunter DJ; OA Biomarkers Consortium.. Predictive validity of biochemical biomarkers in knee osteoarthritis: data from the FNIH OA Biomarkers Consortium. Ann Rheum Dis. 2017 Jan;76(1):186-195. doi: 10.1136/annrheumdis-2016-209252. Epub 2016 Jun 13. PubMed PMID: 27296323; PubMed Central PMCID: PMC5851287.
- 2 Van Spil WE, Nair SC, Kinds MB, Emans PJ, Hilberdink WK, Welsing PM, Lafeber FP. Systemic biochemical markers of joint metabolism and inflammation in relation to radiographic parameters and pain of the knee: data from CHECK, a cohort of early-osteoarthritis subjects. Osteoarthritis Cartilage. 2015 Jan;23(1):48-56. doi: 10.1016/j.joca.2014.09.003. Epub 2014 Sep 6. PubMed PMID: 25205017.