Pain and stiffness due to arthritis in a hand(s) can affect a person’s ability to do everything from preparing meals to using a cell phone. Recognizing the symptoms of hand osteoarthritis and obtaining an accurate diagnosis are the first steps to getting treatment and making everyday tasks easier.
Hand pain and stiffness are the two most common symptoms caused by hand osteoarthritis.
In This Article:
- When Hand Pain Is Osteoarthritis
- Risk Factors for Hand Osteoarthritis
- Recognizing Osteoarthritis in the Hand
- Treatments for Osteoarthritis in Hands
Symptoms of Osteoarthritis of the Hand
There are several key signs and symptoms practitioners look for when diagnosing osteoarthritis in the fingers and wrists:
Pain and stiffness
People with hand arthritis often complain of localized pain in the thumbs, knuckles (DIP/PIP), and/or wrists. Stiffness may be worse after periods of inactivity. Everyday tasks such as using a smartphone or buttoning a shirt may become more difficult to perform.
Hand weakness
A person with hand osteoarthritis may notice that the affected hand(s) seems weaker than it was before osteoarthritis symptoms occurred. Gripping and pinching objects may be more difficult. For example, a person may have trouble opening jars or turning the ignition key of a car.
Carpal tunnel syndrome
When arthritis changes the bony and soft tissue structures in the wrist, an area within the wrist called the carpal tunnel can shrink, becoming narrower. As the tunnel shrinks, it squeezes the nerve that travels through it, causing numbness and/or tingling in the thumb, index finger, long finger, and half of the ring finger.
Read Is My Hand and Wrist Pain Caused by Carpal Tunnel Syndrome or Something Else? on Sports-health.com
Bouchard’s nodes
These bony growths develop in the middle knuckle (PIP joint), making the knuckle look bigger or swollen. Bouchard’s nodes can make it difficult to get a ring on and off a finger.
Heberden’s nodes
Like Bouchard’s nodes, Heberden’s nodes are bony growths that develop in the end-most knuckle (DIP joint).
Knobby-looking thumb
People who have osteoarthritis at the basilar joint of their thumbs may notice the base of the thumb looks “knobby” or “squared off.” This is a sign that bony growths have developed on the bones of the joint.
If hand pain comes on suddenly, it is more likely to be caused by trauma or another condition, not by osteoarthritis. If fingers, palms, and/or wrists feel hot or the skin around a joint turns red, then osteoarthritis is probably not the culprit. An infection, rheumatoid arthritis, or another condition may be the cause, and consultation with a medical professional is advised.
Read more about Osteoarthritis Symptoms and Signs
Diagnosing Osteoarthritis of the Hand
There is no single test for osteoarthritis of the hand. Rather, doctors use several approaches to decide whether hand symptoms are caused by osteoarthritis or something else.
The diagnostic process begins with a patient interview and clinical evaluation, and may involve medical imaging and clinical testing:
Patient interview
The doctor will ask the person about which joints hurt, what activities make the pain worse, and how long they have been experiencing symptoms. Some patients may be asked to fill out a questionnaire about how pain affects their everyday activities. The doctor may also ask if the patient has a family history, previous injury, or job that puts him or her at higher risk for hand osteoarthritis.
Clinical evaluation
Just looking at the hands can give a doctor an idea of whether or not a person has osteoarthritis. Indicators include Bouchard’s nodes, Heberden’s nodes, and/or a knobby-looking thumb (described above).
The doctor will also try to trigger pain by palpating the hands—feeling them and pressing on certain areas—and asking the patient to do certain tasks, such as grasping an object.
Medical imaging
Diagnosing hand osteoarthritis does not require medical imaging. When medical imaging is ordered, it is typically because the doctor wants to rule out another condition or wants to assess the severity of the osteoarthritis damage in the hand.
There are three types of medical imaging that can be used to detect hand osteoarthritis.
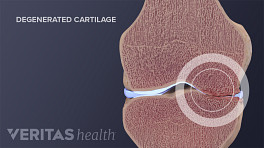
- X-rays can show bone abnormalities, such as the development of bony growths (called bone spurs or osteophytes) and the loss of joint space between bones, which is caused by the loss of articular cartilage. Most bone abnormalities can be observed during a physical examination of the hand, so x-rays are not necessarily helpful for diagnosing arthritis. 1 Marshall M, Watt FE, Vincent TL, Dziedzic K. Hand osteoarthritis: clinical phenotypes, molecular mechanisms and disease management. Nat Rev Rheumatol. 2018;14(11):641‐656. doi:10.1038/s41584-018-0095-4
- Ultrasound imaging may be used to detect changes and inflammation in the hand joints. This imaging technology is particularly useful to rule out inflammatory arthritis, such as rheumatoid arthritis. Ultrasound is relatively inexpensive and can be done in the doctor’s office, but using it correctly requires special medical training.
- Magnetic resonance imaging (MRI) shows detailed 3D imaging of the ligaments, tendons, synovial membrane, and other tissues. It can also detect certain changes to the bone, such as bone cysts. MRI is more expensive and time-consuming than x-rays and ultrasounds.
Researchers estimate that more than 20% of people in the US have some signs of hand osteoarthritis on x-rays, most of them older. 1 Marshall M, Watt FE, Vincent TL, Dziedzic K. Hand osteoarthritis: clinical phenotypes, molecular mechanisms and disease management. Nat Rev Rheumatol. 2018;14(11):641‐656. doi:10.1038/s41584-018-0095-4
Lab testing
There are no lab tests that confirm osteoarthritis in the hand. However, a doctor may order lab tests to rule out other possible causes of hand pain, such as rheumatoid arthritis or psoriatic arthritis.
Many people experience hand pain and stiffness. Recognizing these symptoms and getting a diagnosis can lead to an individual treatment plan that makes day-to-day living easier and less painful.
- 1 Marshall M, Watt FE, Vincent TL, Dziedzic K. Hand osteoarthritis: clinical phenotypes, molecular mechanisms and disease management. Nat Rev Rheumatol. 2018;14(11):641‐656. doi:10.1038/s41584-018-0095-4