Pain and tenderness at the outward curve of the upper thigh can be a sign of hip bursitis. Hip bursitis occurs when the large bursa that lies over the bony knob near the top of the thighbone (medically known as the femur bone’s greater trochanter) becomes inflamed.
As symptoms progress, pain may radiate down the outside of the thigh and occasionally to the buttock, groin, knee, and low back. It may be painful to walk, climb up stairs, lie down on the side of the affected hip, or get out of a chair, especially after sitting for a long time. Pain when lying on one’s side is one of the most obvious signs of trochanteric bursitis, however, this symptom may not always be present.
In This Article:
- Hip (Trochanteric) Bursitis
- Hip Bursitis Symptoms
- Hip Bursitis Causes
- Hip Bursitis Diagnosis
- Hip Bursitis Treatment
- Hip Bursitis Video
Hip Bursa and Bursitis
Before learning about hip bursitis, it is helpful to know about bursae and bursitis.
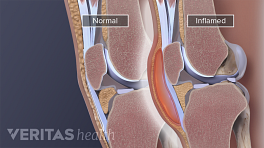
- A bursa is a thin, slippery sac filled with a small amount of fluid. The bursa’s outer membrane, called a synovial membrane or synovium, produces and contains synovial fluid.
The purpose of a healthy bursa is to reduce friction between bone and surrounding soft tissue, such as skin, muscles, ligaments and tendons. There are more than 140 bursae in the body, 1 Azar FM, Beaty JH, Canale TS, eds. Campbell’s Operative Othopaedics, 13th ed., vol 1, page 482. Philadelphia PA: Elsevier; 2017. several of which are found near the hip joint.
- Bursitis occurs when a bursa’s synovial membrane becomes irritated and inflamed. The inflamed membrane may produce excess synovial fluid, causing the bursa to swell. Hip bursae are located underneath skin, fat, muscle, and other soft tissues, so even moderate to severe swelling may not be apparent.
The hip bursa that is most prone to bursitis is the trochanteric bursa.
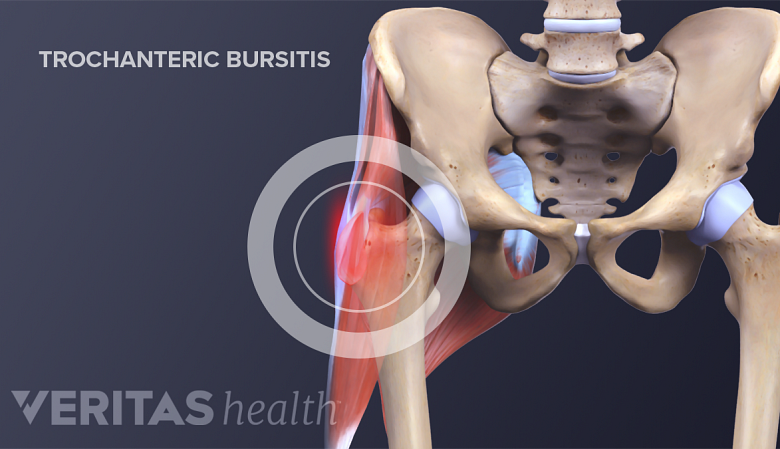
Trochanteric Bursitis
Trochanteric bursitis is one of the two most common forms of hip bursitis. It affects the greater trochanteric bursa which is located at the outward curve of the upper thigh.
The greater trochanter is the bony knob near the top of the thighbone (femur), where the upper thigh curves outward. The trochanteric bursa is located over this bony knob. It provides a cushion and reduces friction between the bone’s surface and the soft tissue (Iliotibial band) that runs over it during hip and knee movement.
When the trochanteric bursa becomes inflamed, it is called trochanteric bursitis, or hip bursitis. The trochanteric bursa typically becomes inflamed because of:
- An injury, such as a fall or other form of direct impact, causing the bursa to fill with blood (called a hematoma). The blood may irritate the bursa and cause inflammation.
- Repeated friction in the hip joint. For example, friction can occur when a too-tight iliotibial band (IT band) travels back and forth over the hip’s trochanteric bursa during knee and hip movement.
- Excessive pressure over the outside of the hip can also cause trochanteric bursitis, such as sleeping on a hard surface while camping. You may notice a significant tenderness over the outside of the thigh the next morning.
- Tears or inflammation in the gluteus medius tendon. Tendonitis is the abductor tendons are linked to the development of trochanteric bursitis.
Trochanteric bursitis causes pain at the outside of the hip.
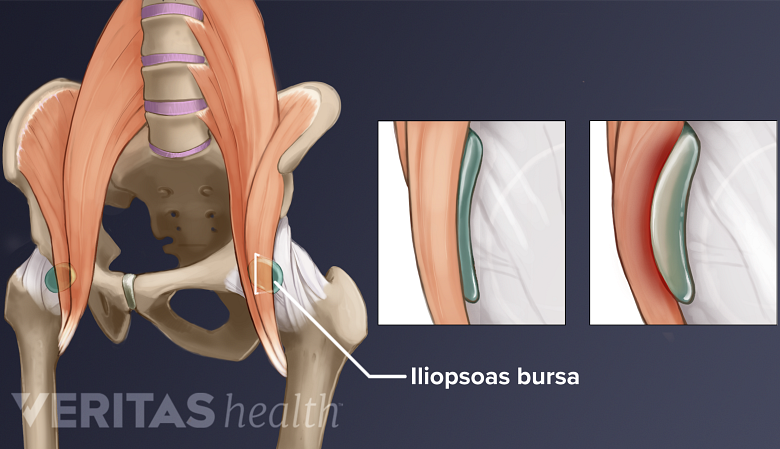
Iliopsoas Bursitis
Iliopsoas bursitis is inflammation of the smaller iliopsoas bursa.
In addition to the trochanteric bursa, there are other bursa located near the hip joint. One of them, called the iliopsoas bursa, is located near the groin, under the iliopsoas muscle. If this bursa becomes irritated, the condition is called iliopsoas bursitis or iliopectineal bursitis. This condition is also generally referred to as hip bursitis.
The main difference between iliopsoas bursitis and trochanteric bursitis is that iliopsoas bursitis causes pain in front of the hip and/or groin area, while trochanteric bursitis causes pain in the outer hip.
Diagnosis and treatment for the two types of bursitis are similar. This article focuses mainly on trochanteric bursitis, which is more common.
See why the complex hip joint structure is susceptible to arthritic conditions. Read more about Hip Anatomy
Greater Trochanter Pain Syndrome
Tenderness at the outside of the hip may be referred to as greater trochanter pain syndrome 2 Segal NA, Felson DT, Torner JC, et al. Greater trochanteric pain syndrome: epidemiology and associated factors. Arch Phys Med Rehabil. 2007;88(8):988–992. doi:10.1016/j.apmr.2007.04.014 . The terms hip bursitis and greater trochanter pain syndrome may be used synonymously. 3 Haviv B. Update on trochanteric bursitis of the hip. OA Orthopaedics 2013 Jul 13;1(1):10. , 4 Seidman AJ, Varacallo M. Trochanteric Bursitis. 2019 Jan;. Review. PubMed PMID: 30860738. However, a recent study 5 Long SS, Surrey DE, Nazarian LN. Sonography of greater trochanteric pain syndrome and the rarity of primary bursitis. AJR Am J Roentgenol. 2013 Nov;201(5):1083-6. doi: 10.2214/AJR.12.10038. PubMed PMID: 24147479. suggests that hip bursitis affects only about 20% of people diagnosed with greater trochanter pain syndrome.
Other common causes of this syndrome include tightness of the iliotibial band (IT band) and injury to a gluteal tendon. 2 Segal NA, Felson DT, Torner JC, et al. Greater trochanteric pain syndrome: epidemiology and associated factors. Arch Phys Med Rehabil. 2007;88(8):988–992. doi:10.1016/j.apmr.2007.04.014 , 5 Long SS, Surrey DE, Nazarian LN. Sonography of greater trochanteric pain syndrome and the rarity of primary bursitis. AJR Am J Roentgenol. 2013 Nov;201(5):1083-6. doi: 10.2214/AJR.12.10038. PubMed PMID: 24147479. Greater trochanter pain syndrome can have more than one cause.
Septic Hip Bursitis
Septic hip bursitis, in which a bursa in the hip area is infected, is rare. 6 Novatnack ES, Protzman NM, Weiss CB. Primary Septic Greater Trochanteric Bursitis. J Glob Infect Dis. 2015;7(2):93–94. doi:10.4103/0974-777X.154448 It is a potentially serious condition that requires medical attention and treatment with antibiotics.
Septic hip bursitis will cause similar symptoms as aseptic (non-infectious) bursitis as well as fatigue, fever, warmth and redness at the hip, and/or an overall feeling of being ill. Recognizing the symptoms of septic bursitis can lead to quick and appropriate treatment.
See Septic Bursitis
- 1 Azar FM, Beaty JH, Canale TS, eds. Campbell’s Operative Othopaedics, 13th ed., vol 1, page 482. Philadelphia PA: Elsevier; 2017.
- 2 Segal NA, Felson DT, Torner JC, et al. Greater trochanteric pain syndrome: epidemiology and associated factors. Arch Phys Med Rehabil. 2007;88(8):988–992. doi:10.1016/j.apmr.2007.04.014
- 3 Haviv B. Update on trochanteric bursitis of the hip. OA Orthopaedics 2013 Jul 13;1(1):10.
- 4 Seidman AJ, Varacallo M. Trochanteric Bursitis. 2019 Jan;. Review. PubMed PMID: 30860738.
- 5 Long SS, Surrey DE, Nazarian LN. Sonography of greater trochanteric pain syndrome and the rarity of primary bursitis. AJR Am J Roentgenol. 2013 Nov;201(5):1083-6. doi: 10.2214/AJR.12.10038. PubMed PMID: 24147479.
- 6 Novatnack ES, Protzman NM, Weiss CB. Primary Septic Greater Trochanteric Bursitis. J Glob Infect Dis. 2015;7(2):93–94. doi:10.4103/0974-777X.154448