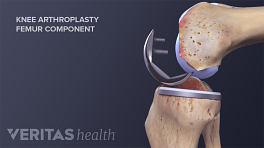
Not all knee replacement surgeries are the same. The size and location of the incision can vary, and the surgeon may use different tools and technologies to perform the surgery. The artificial knee components can also vary—for example, components may be standard, gender-specific, custom-made, or composed of non-traditional material(s), such as ceramic.
In This Article:
- Total Knee Replacement: Facts and Considerations for Patients
- Knee Replacement Components: Options for Patients
Potential variables in knee replacement surgery are discussed in this article. These variables, in addition to the surgeon’s experience and the patient’s overall health and knee anatomy, may affect post-surgical improvements in pain and knee function.
See Questions to Ask Before Knee Replacement
Minimally Invasive Knee Replacement Surgery
The goal of minimally invasive surgery is to preserve more muscle and other soft tissue around the knee, helping facilitate a faster and better recovery. A minimally invasive surgery uses a 3 to 6-inch incision, compared to an 8 to 12-inch incision for a traditional surgery. In addition, the knee cap is typically not disturbed and many soft tissues are pushed aside—rather than cut—to make room for the surgical procedure.
See Traditional Knee Replacement vs. Minimally Invasive Knee Replacement
Minimally invasive knee replacement has become less popular in recent years. 1 Picard F, Deakin A, Balasubramanian N, Gregori A. Minimally invasive total knee replacement: techniques and results. European Journal of Orthopaedic Surgery & Traumatology. 2018;28(5):781-791. doi:10.1007/s00590-018-2164-4. Less invasive surgical approaches are technically challenging surgeries and carry their own, different set of risks. For example, less invasive surgeries seem to have a higher risk of post-surgical alignment problems 2 Dalury DF, Dennis DA. Mini-incision total knee arthroplasty can increase risk of component malalignment. Clin Orthop Relat Res. 2005;440:77–81. and nerve damage. 3 Gandhi R, Smith H, Lefaivre KA, Davey JR, Mahomed NN. Complications after minimally invasive total knee arthroplasty as compared with traditional incision techniques: a meta-analysis. J Arthroplasty. 2011;26(1):29–35.
See The Pros and Cons of Minimally Invasive Knee Replacement Surgery
Computer-assisted Knee Replacement Surgery
Computer-assisted knee replacement surgery is not common in the United States, perhaps because of its cost and the time it adds on to surgery. However, some studies suggest that computer-assisted surgery may provide better implant positioning and better alignment. 4 Mason JB, Fehring TK, Estok R, Banel D, Fahrbach K. Meta-analysis of alignment outcomes in computer-assisted total knee arthroplasty surgery. J Arthroplasty. 2007;22(8):1097–106. doi: 10.1016/j.arth.2007.08.001. One study comparing nearly 200 surgeries found that people who had computer assisted surgery had better knee function 5 years after surgery. 5 Mihalko, WM. Arthroplasty of the Knee. In: Azar FM, Beaty JH, Canale ST, eds. Campbell’s Operative Orthopaedics, 13th ed. Philidelphia, PA. Elsevier. 2017:396-468.
Computer assistance may be especially useful for prostheses alignment in patients who are bowlegged. 6 Chauhan SK, Scott RG, Breidahl W, Beaver RJ. Computer-assisted knee arthroplasty versus a conventional jig-based technique. A randomised, prospective trial. J Bone Joint Surg Br. 2004 Apr;86(3):372-7. PubMed PMID: 15125124. Accessed January 18, 2012, http://web.jbjs.org , 7 Computer-Assisted Knee Arthroplasty Is Better Than a Conventional Jig-Based Technique in Terms of Component Alignment. The Journal of Bone & Joint Surgery. 2004; 86:2573-2573, Accessed, January 31, 2012, http://www.jbjs.org , 8 Huang TW, Hsu WH, Peng KT, Hsu RW, Weng YJ, Shen WJ. Total knee arthroplasty with use of computer-assisted navigation compared with conventional guiding systems in the same patient: radiographic results in Asian patients. J Bone Joint Surg Am. 2011 Jul 6;93(13):1197-202. PubMed PMID: 21776572
Patients will want to consider these options but keep in mind a surgeon’s experience remains one of the most important factors. Certain surgical techniques and technologies have steep learning curves for surgeons. An experienced surgeon who uses a traditional surgical approach may offer better outcomes than a less experienced surgeon who is using the latest technology and methods.
Outpatient (Same Day) Knee Replacement
People who undergo outpatient knee replacement are discharged the same day they have surgery. Some evidence suggest that outpatient knee replacement surgery saves money and offers the same or better results for eligible patients, though more study is needed. 9 Lazic S, Boughton O, Kellett CF, Kader DF, Villet L, Rivière C. Day-case surgery for total hip and knee replacement: How safe and effective is it? EFORT Open Reviews. 2018;3(4):130-135. doi:10.1302/2058-5241.3.170031.
See The Advantages and Disadvantages of Outpatient Knee Replacement
Outpatient knee replacement is relatively uncommon. Many patients have other conditions, such as heart disease, that justify one or more nights of post-surgical observation at the hospital. 10 Lovald S, Ong K, Lau E, Joshi G, Kurtz S, Malkani A. Patient selection in outpatient and short-stay total knee arthroplasty. J Surg Orthop Adv. 2014 Spring;23(1):2-8. PubMed PMID: 24641891. In addition, many surgeons and patients simply prefer at least one night of post-surgical observation.
- 1 Picard F, Deakin A, Balasubramanian N, Gregori A. Minimally invasive total knee replacement: techniques and results. European Journal of Orthopaedic Surgery & Traumatology. 2018;28(5):781-791. doi:10.1007/s00590-018-2164-4.
- 2 Dalury DF, Dennis DA. Mini-incision total knee arthroplasty can increase risk of component malalignment. Clin Orthop Relat Res. 2005;440:77–81.
- 3 Gandhi R, Smith H, Lefaivre KA, Davey JR, Mahomed NN. Complications after minimally invasive total knee arthroplasty as compared with traditional incision techniques: a meta-analysis. J Arthroplasty. 2011;26(1):29–35.
- 4 Mason JB, Fehring TK, Estok R, Banel D, Fahrbach K. Meta-analysis of alignment outcomes in computer-assisted total knee arthroplasty surgery. J Arthroplasty. 2007;22(8):1097–106. doi: 10.1016/j.arth.2007.08.001.
- 5 Mihalko, WM. Arthroplasty of the Knee. In: Azar FM, Beaty JH, Canale ST, eds. Campbell’s Operative Orthopaedics, 13th ed. Philidelphia, PA. Elsevier. 2017:396-468.
- 6 Chauhan SK, Scott RG, Breidahl W, Beaver RJ. Computer-assisted knee arthroplasty versus a conventional jig-based technique. A randomised, prospective trial. J Bone Joint Surg Br. 2004 Apr;86(3):372-7. PubMed PMID: 15125124. Accessed January 18, 2012, http://web.jbjs.org
- 7 Computer-Assisted Knee Arthroplasty Is Better Than a Conventional Jig-Based Technique in Terms of Component Alignment. The Journal of Bone & Joint Surgery. 2004; 86:2573-2573, Accessed, January 31, 2012, http://www.jbjs.org
- 8 Huang TW, Hsu WH, Peng KT, Hsu RW, Weng YJ, Shen WJ. Total knee arthroplasty with use of computer-assisted navigation compared with conventional guiding systems in the same patient: radiographic results in Asian patients. J Bone Joint Surg Am. 2011 Jul 6;93(13):1197-202. PubMed PMID: 21776572
- 9 Lazic S, Boughton O, Kellett CF, Kader DF, Villet L, Rivière C. Day-case surgery for total hip and knee replacement: How safe and effective is it? EFORT Open Reviews. 2018;3(4):130-135. doi:10.1302/2058-5241.3.170031.
- 10 Lovald S, Ong K, Lau E, Joshi G, Kurtz S, Malkani A. Patient selection in outpatient and short-stay total knee arthroplasty. J Surg Orthop Adv. 2014 Spring;23(1):2-8. PubMed PMID: 24641891.