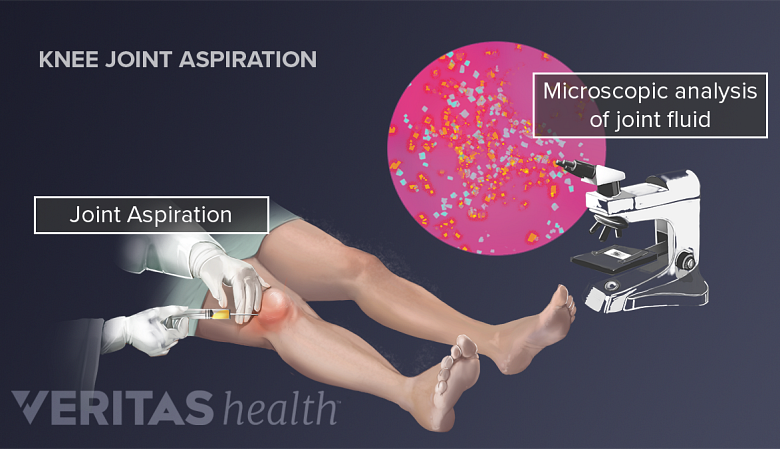
Analyzing the fluid from a joint or bursa can help a doctor identify the underlying cause of inflammation and swelling. It can be an important step to help rule out or support the diagnosis of gout, rheumatoid arthritis, infection, or other condition.
Fluid from joint aspiration can be analyzed to aid in the diagnostic process.
Fluid is collected from a joint using a needle and syringe in a procedure commonly called arthrocentesis, or joint aspiration. When fluid is removed from a bursa it is called bursal aspiration. A doctor will decide what types of fluid analyses should be performed based on the patient’s symptoms and health history.
Four common types of fluid analyses are described below.
In This Article:
- What Is Arthrocentesis (Joint Aspiration)?
- The Joint Aspiration Procedure
- Arthrocentesis Recovery and Potential Risks
- Diagnosis through Synovial Fluid Analysis
1. Physical and Visual Examination
The synovial fluid sample will be checked for certain features. Below are some characteristics that can be assessed before a more scientific analysis is done.
- Fluid volume may be greater than normal. Joints and bursae normally contain very small amounts of synovial fluid—sometimes less than 1 mL, 1 Mundt L, Shanahan K MS MT(ASCP), Graf’s Textbook of Routine Urinalysis and Body Fluids (p.255), Philadelphia, Pa: Lippincott Williams & Wilkins; 2011 depending on the size of the joint. An inflamed joint or bursa may contain several times the normal amount of fluid.
- Viscosity may be decreased. Normal synovial fluid is viscous and often compared to egg whites. Inflammation may cause synovial fluid to be less viscous.
- Color and clarity may vary. Normal synovial fluid is clear and colorless or straw-colored. Abnormal fluid may look cloudy, opaque, and/or differently colored. For example, cloudy fluid may indicate an infection, and pink or reddish fluid may indicate the presence of blood.
Variations in the fluid’s volume, viscosity, color, or clarity may indicate the need for further lab testing.
2. Microscopic Analysis
A specially trained lab technician will prepare a synovial fluid sample and examine it under a microscope for crystals, white blood cell count, microorganisms, and possible unusual traits.
- Crystals are not seen in normal synovial fluid. The presence of uric acid crystals in the synovial fluid indicates gout. The presence of calcium pyrophosphate crystals in synovial fluid indicates pseudogout. (A trained lab technician can determine the crystal type by its size, shape, and how it refracts light.)
- A white blood cell count that is higher than normal may indicate infectious arthritis, gout, or rheumatoid arthritis. For example, results that show more than 50,000 WBC µL (white blood cells per cubic millimeter) may indicate a bacterial infection. 2 Seidman AJ, Limaiem F. Synovial Fluid Analysis. [Updated 2019 Jan 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537114/
- Microorganisms, typically bacteria, indicate infection and can sometimes be detected under a microscope, and typically this can be verified with a culture study.
- Red blood cell counts may be high after a traumatic injury and slightly elevated in patients with osteoarthritis. They may also be present if the patient has a bleeding disorder, such as hemophilia.
It is possible to find uric acid crystals and microbiota in the same joint fluid sample, indicating both gout and an infection are present. 2 Seidman AJ, Limaiem F. Synovial Fluid Analysis. [Updated 2019 Jan 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537114/
3. Chemical Analysis
Assessment of the chemical make-up of the synovial fluid can be helpful for an arthritis diagnosis. This analysis is typically done by a lab technician who reports the results to the physician’s office.
Below are examples of common types of synovial fluid chemical analysis.
- Uric acid content may be higher than normal for people with gout.
- Glucose levels that are lower than normal may indicate infection. Slightly low glucose levels are also sometimes seen in rheumatoid arthritis.
- Lactate dehydrogenase (LDH), an enzyme normally found in synovial fluid, might be at elevated levels in people who have rheumatoid arthritis, infectious arthritis, or gout.
- Protein levels that are higher than normal may indicate an infection.
A diagnosis supported by abnormal chemical analysis results may require additional evidence, such as information from bloodwork and physical exam.
4. Cultures and Gram Stains
Bacteria and fungi are not normally seen in healthy synovial fluid, and their presence indicates an infection. Microbiologic studies such as cultures and Gram stains can be performed on synovial fluid samples to detect and identify microorganisms.
A doctor may order other lab tests not listed above to further ascertain the fluid’s composition and help make or rule out certain diagnoses.
Lab tests are not infallible, and doctors do not use lab test results alone to make a diagnosis. Rather, these results are used in conjunction with information gathered from a physical examination, patient interview, and other sources, such as x-rays.
Results are usually available to patients within 1 to 3 days. In an urgent situation, lab tests might be expedited and results will be available sooner.
- 1 Mundt L, Shanahan K MS MT(ASCP), Graf’s Textbook of Routine Urinalysis and Body Fluids (p.255), Philadelphia, Pa: Lippincott Williams & Wilkins; 2011
- 2 Seidman AJ, Limaiem F. Synovial Fluid Analysis. [Updated 2019 Jan 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537114/