Before making a diagnosis of shoulder bursitis or shoulder impingement, a doctor must rule out other common problems that could cause shoulder pain.
To identify the root cause of shoulder pain, a doctor may use medical imaging, a diagnostic injection, and/or lab tests. These diagnostic tools can be helpful when used in combination with a patient interview and physical exam.
In This Article:
Medical Imaging
A doctor may order medical imaging to help diagnose or rule out causes of the patient’s symptoms. Medical imaging may include one or more of the following:
- X-ray, which can show signs of osteoarthritis in the shoulder’s glenohumeral (ball-and-socket) and acromioclavicular joints. It can also show certain bony abnormalities, such as a curved or hooked acromion, that increase the likelihood of shoulder impingement.
- Magnetic resonance imaging (MRI), which can show detailed images of bone tissue as well as soft tissues, such as the rotator cuff, biceps tendon, and bursa.
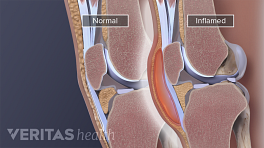
- Ultrasound, which can detect a thickened bursal membrane and excess synovial fluid in a swollen bursa.
Medical imaging is not necessarily required for and accurate diagnosis. In addition, patients should keep in mind that most people over the age of 40 have some degeneration in their shoulder joint. This degeneration is not always painful and does not always require treatment.
Anesthetic Injection
If injecting lidocaine under the shoulder's acromion relieves pain, it likely indicates shoulder impingement.
One way to tell if the pain is related to shoulder impingement syndrome is to inject an anesthetic called lidocaine hydrochloride into the subacromial space, under the shoulder’s acromion. This location is where soft tissues get pinched during shoulder impingement. If the injection relieves the pain, impingement syndrome is the likely cause.
Aspiration and Lab Tests
A doctor may perform an aspiration, removing fluid from the shoulder’s bursa with a needle and syringe. In addition to relieving pressure and making the patient more comfortable, aspiration provides a fluid sample that can be tested for infection. Aspiration of the shoulder bursa is less common than it is in knee and elbow bursae, which are more prone to severe swelling and septic bursitis.
Blood tests may also be used to help rule out or confirm systemic (body-wide) infection and inflammatory conditions, such as rheumatoid arthritis, psoriatic arthritis, and polymyalgia rheumatica. These conditions can cause joint pain and increase the likelihood developing bursitis, including shoulder bursitis.