Featured Health Topics
Shoulder Osteoarthritis Symptoms
Pain and stiffness at the back of the shoulder is a major symptom of shoulder osteoarthritis. Other signs include shoulder impingement and crepitus.
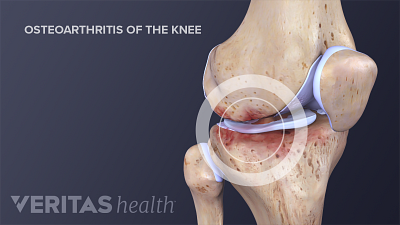
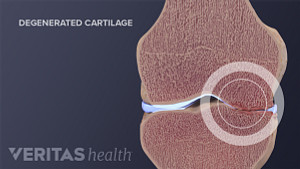
Knee Osteoarthritis Symptoms
Knee osteoarthritis symptoms can vary widely. Recognizing these symptoms early on can speed up treatment and help prevent symptoms from getting worse.
Trigger Finger (Stenosing Tenosynovitis)
Trigger finger, also known as stenosing tenosynovitis, occurs when the fingers' tendon sheaths become inflamed, often in patients with rheumatoid arthritis.
Stem Cell Therapy for Arthritis
Spotlight on your health
Rheumatoid Arthritis Overview Video
Over 2 million Americans, or 1% of the population, are living with rheumatoid arthritis. Learn the symptoms of this autoimmune disorder and chronic type of inflammatory arthritis.
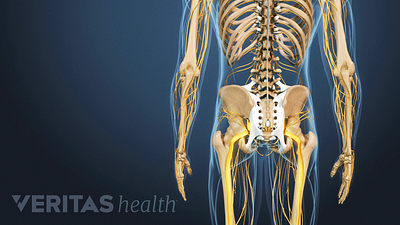
Ankylosing Spondylitis Treatment
Medications that decrease inflammation are used to treat ankylosing spondylitis, and physical therapy and exercise help reduce pain and improve mobility.
Shoulder Osteoarthritis Video
This physician reviewed shoulder osteoarthritis video lays out the symptoms and treatment options for patients with pain from shoulder cartilage degeneration.
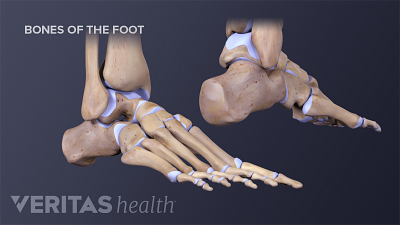
Ankle Osteoarthritis Causes
Ankle osteoarthritis is often preceded by an ankle injury, and may initially feel like the old injury, but there are other determining factors as well.
Editors Top Picks
Treatments for rheumatoid arthritis, such as medication, exercise, and possibly surgery, are aimed to reduce pain, increase joint function, and slow damage.
Joint pain may be a sign of osteoarthritis, which is caused by the breakdown of cartilage and underlying bone in joints such as the hands, knees, hips, and others.
There is no one single cause of psoriatic arthritis. Risk factors range from genetics and certain medical conditions to smoking and food choices.