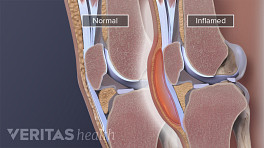
The goal of knee bursitis treatment is to reduce the inflammation that causes knee swelling and other symptoms. While home treatments may work for mild or moderate cases, chronic or severe cases may require medical intervention. Septic knee bursitis—which is caused by an infection—requires urgent medical care and antibiotic therapy.
In This Article:
Home Treatments for Knee Bursitis
It is possible to successfully treat mild to moderate cases of aseptic (non-infectious) knee bursitis at home. People who are not sure if their bursitis is septic or not are advised to consult with a physician.
Home treatments for knee bursitis include:
Rest
Activities that may aggravate the affected prepatellar bursae, such as kneeling, crawling, or participating in high impact sports, should be avoided.
Cold compress
Applying a cold compress to the knee may help decrease swelling and alleviate other symptoms.
A cold compress can be purchased or made at home and applied to the knee for about 20 minutes 2 or 3 times a day. (Homemade compresses that use ice can be wrapped in a towel to prevent injury to the skin.)
See 3 Types of Cold Packs for Arthritis
Non-steroidal anti-inflammatory drugs (NSAIDs)
Over-the-counter non-steroidal anti-inflammatory medications, such as ibuprofen, may reduce knee pain, swelling, and inflammation.
Medical Treatments for Knee Bursitis
When knee swelling and other symptoms do not respond to home treatments within 2 or 3 weeks, or if symptoms of septic bursitis are present, medical treatment is advised.
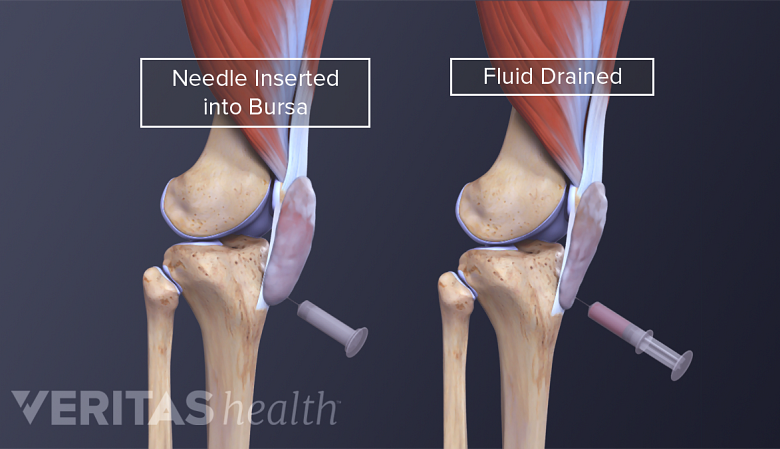
Bursal aspiration
Excess fluid may be removed from the prepatellar bursa using a needle and syringe. This procedure, called bursal aspiration, may relieve pressure in the knee. While aspiration is often effective, it is possible that swelling will return.
Aspiration is also used as a diagnostic tool. The physician may send the aspirated bursa fluid to a lab to be tested for signs of infection or other problems, such as gout.
See What Is Arthrocentesis (Joint Aspiration)?
Cortisone injection
A doctor may recommend a cortisone injection when prepatellar bursitis is associated with another inflammatory condition, such as gout or rheumatoid arthritis. 1 Khodaee M. Common Superficial Bursitis. Am Fam Physician. 2017 Feb 15;95(4):224-231. PMID: 28290630.
Recent research suggests cortisone injections are not an effective treatment for most other cases of prepatellar bursitis.1 In addition, cortisone injections into the prepatellar bursa are associated with side effects, such as skin discoloration, degeneration, and infection near the site of injection. 1 Khodaee M. Common Superficial Bursitis. Am Fam Physician. 2017 Feb 15;95(4):224-231. PMID: 28290630.
Since cortisone may cause tissue damage, newer treatments, including platelet-rich plasma and other regenerative medicine techniques, are sometimes used. The scientific evidence for this type of treatment is ongoing.
Read more about Cortisone Injections (Steroid Injections)
Antibiotic therapy
Septic prepatellar bursitis requires treatment with antibiotics. Oral antibiotics are typically successful when treating mild to moderate septic bursitis. People who show signs of severe infection or who have compromised immune systems may require hospitalization and intravenous antibiotics. 1 Khodaee M. Common Superficial Bursitis. Am Fam Physician. 2017 Feb 15;95(4):224-231. PMID: 28290630.
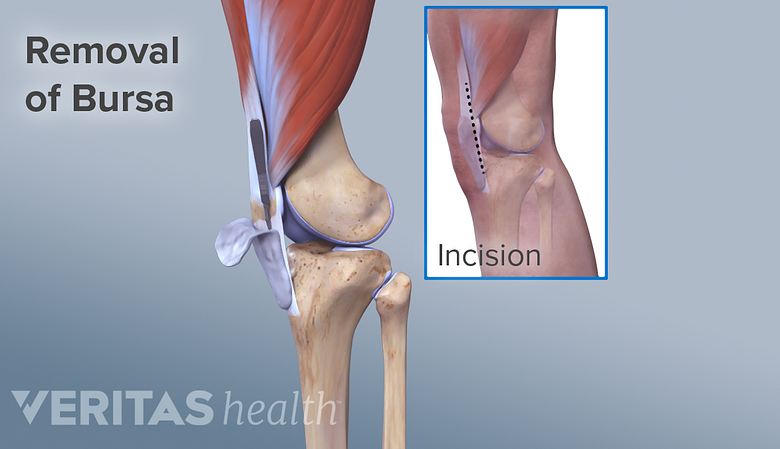
Bursectomy
A septic (infected) or chronic prepatellar bursa may need to be surgically removed.
Challenging cases of chronic or septic knee bursitis may warrant surgery to remove the affected bursae. This surgery is called a bursectomy.
- A traditional bursectomy requires making an incision in the skin over the knee to remove the prepatellar bursa.
- An endoscopic bursectomy uses smaller incisions. This approach may be used to lower the risk of infection, trouble healing, and scarring. 1 Khodaee M. Common Superficial Bursitis. Am Fam Physician. 2017 Feb 15;95(4):224-231. PMID: 28290630.
- Both approaches may be done as in-office or outpatient hospital procedures.
Not all experts agree on when to use bursectomies to treat septic prepatellar bursitis. 1 Khodaee M. Common Superficial Bursitis. Am Fam Physician. 2017 Feb 15;95(4):224-231. PMID: 28290630. , 2 Aaron DL, Patel A, Kayiaros S, Calfee R. Four common types of bursitis: diagnosis and management. J Am Acad Orthop Surg. 2011 Jun;19(6):359-67. doi: 10.5435/00124635-201106000-00006. PMID: 21628647. , 3 Lormeau C, Cormier G, Sigaux J, Arvieux C, Semerano L. Management of septic bursitis. Joint Bone Spine. 2019 Oct;86(5):583-588. doi: 10.1016/j.jbspin.2018.10.006. Epub 2018 Oct 26. PMID: 31615686. Some doctors recommend an immediate bursectomy for all cases. Others cite limited evidence that antibiotic treatment alone is more effective. 1 Khodaee M. Common Superficial Bursitis. Am Fam Physician. 2017 Feb 15;95(4):224-231. PMID: 28290630. , 4 Sayegh ET, Strauch RJ. Treatment of olecranon bursitis: a systematic review. Arch Orthop Trauma Surg. 2014 Nov;134(11):1517-36. doi: 10.1007/s00402-014-2088-3. Epub 2014 Sep 19. PMID: 25234151.
Before a bursectomy, aspiration will be done to remove excess fluid from the bursa. Following a bursectomy or sclerotherapy, a new patellar bursa will likely develop. Prevention strategies can help ensure bursitis does not occur in this new bursa.
Prepatellar Bursitis Recovery Time
Successful nonsurgical treatment of prepatellar bursitis may take 2 weeks or longer. If left untreated, chronic bursitis may last months or years.
Preventing Knee Bursitis
Once successfully treated, certain steps can be taken to prevent knee bursitis from returning and becoming chronic.
Periodic rest
While movement and exercise are essential to overall health, cutting back on activities that irritate the bursa may reduce the chance of a flare-up. Taking periodic breaks from certain activities can also help.
Knee pads
People who spend time on their knees (people who install tile and carpet floors, for example) may benefit from kneepads. Using kneepads can take some pressure off the patella’s bursa.
Treating underlying conditions
If knee bursitis is associated with an underlying medical condition, such as diabetes or gout, then treating the underlying condition will help prevent future flare-ups.
Knee bursitis is usually successfully treated without surgery or injections. It is important to wait until all knee pain and swelling are gone before resuming normal activities. Returning to activities that irritate the prepatellar bursa before it is healed will likely cause the symptoms to flare up again.
Read more about Bursitis Treatment and Prevention
- 1 Khodaee M. Common Superficial Bursitis. Am Fam Physician. 2017 Feb 15;95(4):224-231. PMID: 28290630.
- 2 Aaron DL, Patel A, Kayiaros S, Calfee R. Four common types of bursitis: diagnosis and management. J Am Acad Orthop Surg. 2011 Jun;19(6):359-67. doi: 10.5435/00124635-201106000-00006. PMID: 21628647.
- 3 Lormeau C, Cormier G, Sigaux J, Arvieux C, Semerano L. Management of septic bursitis. Joint Bone Spine. 2019 Oct;86(5):583-588. doi: 10.1016/j.jbspin.2018.10.006. Epub 2018 Oct 26. PMID: 31615686.
- 4 Sayegh ET, Strauch RJ. Treatment of olecranon bursitis: a systematic review. Arch Orthop Trauma Surg. 2014 Nov;134(11):1517-36. doi: 10.1007/s00402-014-2088-3. Epub 2014 Sep 19. PMID: 25234151.