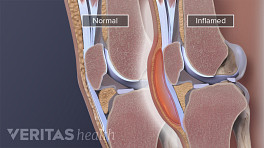
What type of treatment will be recommended for elbow bursitis depends on many factors. If no infection is suspected (aseptic bursitis) then home treatment may be possible. If home treatments do not work, or if there are signs of infection, such as warmth and redness at the elbow, then medical care is advised. Occasionally, surgery to drain and/or remove the elbow’s bursa is recommended.
In This Article:
- Elbow (Olecranon) Bursitis
- Elbow (Olecranon) Bursitis Symptoms
- Elbow (Olecranon) Bursitis Causes
- Elbow (Olecranon) Bursitis Diagnosis
- Elbow (Olecranon) Bursitis Treatment
Nonsurgical Treatments for Elbow Bursitis
Home treatments will be focused on eliminating activities or positions that aggravate the bursa and reducing the inflammation.
R.I.C.E.
Rest, ice, compression, and elevation, known as the R.I.C.E. formula, are often recommended to treat aseptic (not septic) elbow bursitis:
Rest and activity modification
People with elbow bursitis should avoid activities that will aggravate and inflame the bursa and avoid leaning on the elbows or putting any direct pressure on them. Wearing elbow pads can also help protect the elbow bursa from pressure or additional irritation.
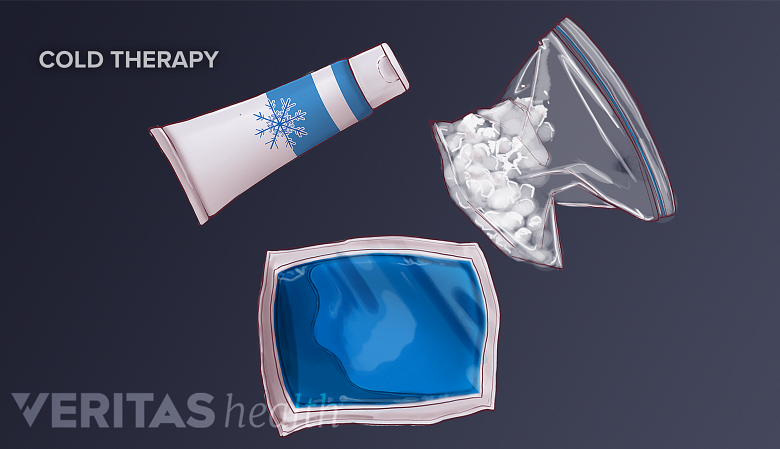
Ice
Cold applied to the elbow may reduce swelling, with time and contact limited to avoid injury.
Applying a cold compress to the swollen elbow two or three times a day may help alleviate symptoms and decrease swelling. To avoid injury to the skin, ice should not be applied directly to the skin and application time should be limited to 10 to 20 minutes.
See When and Why to Apply Cold to an Arthritic Joint
Compression
An elastic compression bandage, such as an Ace brand bandage, wrapped around the affected joint can help control swelling.
Elevation
Keeping the affected elbow at or above the height of the heart can help reduce blood flow to the area, thereby reducing inflammation.
In addition to R.I.C.E., a number of treatments exist to reduce the swelling and any associated pain or discomfort.
Non-steroidal anti-inflammatory drugs (NSAIDs)
Anti-inflammatory medications, such as aspirin, ibuprofen, naproxen, and cox-2 inhibitors (Celebrex) can reduce swelling and inflammation and relieve pain associated with elbow bursitis.
Potential side effects from NSAIDs include gastrointestinal, heart, and kidney problems. 1 Cooper C, Chapurlat R, Al-Daghri N, et al. Safety of Oral Non-Selective Non-Steroidal Anti-Inflammatory Drugs in Osteoarthritis: What Does the Literature Say? Drugs Aging. 2019;36(Suppl 1):15–24. doi:10.1007/s40266-019-00660-1. For this reason, doctors typically do not recommend taking NSAIDs daily for an extended period of time.
Elbow pads
When elbow bursitis has been caused by repeated small traumas—for example, regularly resting weight on the elbow—then wearing elbow pads may be recommended. Elbow pads provide extra cushioning and can be used to help avoid exacerbating existing elbow bursitis symptoms or help prevent bursitis in the future. An elastic compression bandage used to control swelling can provide similar protection.
Antibiotics
Only septic elbow bursitis requires treatment with antibiotics. The choice of antibiotic will likely be influenced by the type of microorganism that is causing the infection. (A bacterium called Staphylococcus aureus is involved in the majority of cases.
2
Zimmermann B 3rd, Mikolich DJ, Ho G Jr. Septic bursitis. Semin Arthritis Rheum 1995;24:391-410. As cited in Reilly D, Kamineni S. Olecranon bursitis. J Shoulder Elbow Surg. 2016 Jan;25(1):158-67. doi: 10.1016/j.jse.2015.08.032. Epub 2015 Nov 11. Review. PubMed PMID: 26577126.
)
Oral antibiotics may be administered promptly and are typically sufficient to treat the infection. However, if the infection is advanced, or if the patient has other complicating factors, antibiotics may be administered intravenously.
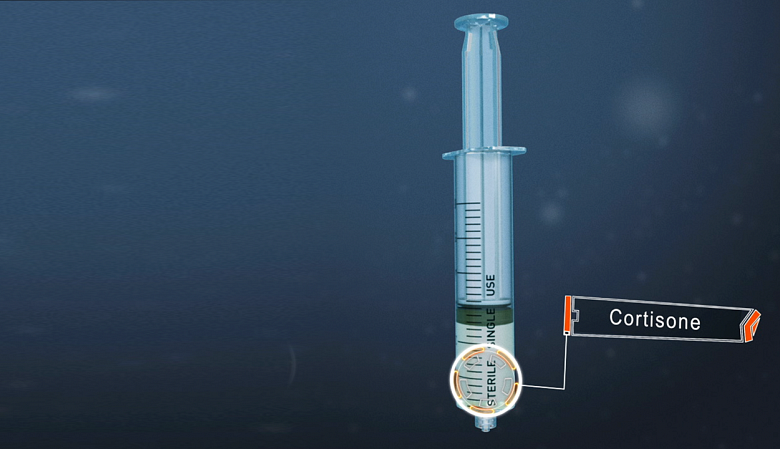
Corticosteroid injection
An injection of cortisone can be useful in treating bursitis by reducing inflammation.
Elbow bursitis symptoms may be quickly relieved with corticosteroid injections. A corticosteroid is a powerful anti-inflammatory medication, and injecting it directly into the inflamed olecranon bursa is usually effective in relieving pain and swelling.
See Cortisone Injections (Steroid Injections)
Corticosteroid injections have potential side effects, such as infection and degeneration of the skin at the elbow. 3 Weinstein PS, Canoso JJ, Wohlgethan JR, "Long-term follow-up of corticosteroid injection for traumatic olecranon bursitis," Ann Rheum Dis, 1984 Feb;43(1):44-6. PubMed PMID: 6696516; PubMed Central PMCID: PMC1001216. , 4 Brinks A, Koes BW, Volkers AC, Verhaar JA, Bierma-Zeinstra SM, "Adverse effects of extra-articular corticosteroid injections: a systematic review," BMC Musculoskelet Disord, 2010 Sep 13;11:206. Review. PubMed PMID: 20836867; PubMed Central PMCID: PMC2945953. , 5 Soderquist B, Hedstrom SA. Predisposing factors, bacteriology and antibiotic therapy in 35 cases of septic bursitis. Scand J Infect Dis 1986;18:305-11. As cited in Reilly D, Kamineni S. Olecranon bursitis. J Shoulder Elbow Surg. 2016 Jan;25(1):158-67. doi: 10.1016/j.jse.2015.08.032. Epub 2015 Nov 11. Review. PubMed PMID: 26577126. Therefore, these injections are usually limited to one or two injections at least one month apart. It is important to perform a corticosteroid injection under ultrasound guidance to ensure proper placement of the medication and avoid injecting corticosteroid into a tendon, which can weaken it. 6 Barnett J, Bernacki MN, Kainer JL, Smith HN, Zaharoff AM, Subramanian SK. The effects of regenerative injection therapy compared to corticosteroids for the treatment of lateral Epicondylitis: a systematic review and meta-analysis. Arch Physiother. 2019;9:12. Published 2019 Nov 13. doi:10.1186/s40945-019-0063-6 , 7 Taylor SA, Hannafin JA. Evaluation and management of elbow tendinopathy. Sports Health. 2012;4(5):384–393. doi:10.1177/1941738112454651
See Cortisone Injection Risks and Side Effects
Platelet-rich plasma injections
Some doctors believe elbow bursitis symptoms may be relieved with an injection of platelet-rich plasma (PRP). PRP is a natural substance composed of platelets from the patient’s own blood. Platelets release proteins called growth factors, substances that help tissue heal after injury. For this treatment, a small amount of blood is drawn from the patient’s arm and the blood is put in a centrifuge, where it is spun at intensely high speeds. The spinning causes the blood to separate into layers, including a thin layer of with a high concentration of platelets. The platelets are then injected into the bursa under ultrasound guidance to ensure proper placement.
See Platelet-Rich Plasma (PRP) Therapy for Arthritis
While many doctors offer this treatment, there is currently no published research that specifically focuses on PRP and elbow bursitis. PRP is not considered a standard treatment and may not be covered by insurance.
See Potential Pros and Cons of PRP Injections
Aspiration to drain the elbow bursa
When a bursa is inflamed and swollen, a doctor may remove the bursa’s fluid with a needle and syringe. This process, called needle aspiration, may be recommended to:
- Immediately relieve pressure and discomfort
- Get a fluid sample to test for an infection
See What Is Arthrocentesis (Joint Aspiration)?
It is possible for a needle aspiration of the elbow’s bursa to trigger or spread an infection, 8 Blackwell JR, Hay BA, Bolt AM, Hay SM. Olecranon bursitis: a systematic overview. Shoulder Elbow 2014;6:182-90. http://dx.doi. org/10.1177/1758573214532787. particularly if there is a skin infection or wound at the site of the needle insertion. If a needle aspiration is not possible, a doctor may recommend making an incision in the skin and draining the bursa (a minor surgical procedure).
Surgery for Elbow Bursitis
Rarely, chronic elbow bursitis or septic elbow bursitis is treated with surgery. A surgeon will make an incision at the elbow and perform one or more procedures:
- Incision and drainage. An incision is made into the inflamed bursa and the bursa’s contents will be drained. This procedure is typically done only when septic bursitis is suspected and if aspiration is not possible. 9 Raddatz DA, Hoffman GS, Franck WA. Septic bursitis: presentation, treatment and prognosis. J Rheumatol 1987; 14: 1160–1163. As cited in Blackwell JR, Hay BA, Bolt AM, Hay SM. Olecranon bursitis: a systematic overview. Shoulder Elbow. 2014;6(3):182–190. doi:10.1177/1758573214532787
- Bursectomy. The bursa is drained and then removed, a procedure called bursectomy or bursa resection. Several months following a bursectomy, a new bursa will usually grow back in place of the one that was removed, so protecting the elbow will continue to be necessary.
- Osteotomy. The surgeon may remove bone spurs that have developed on the elbow. This procedure is called osteotomy (the cutting of bone). Bone spurs are common in people over age 50 and are not a cause for concern on their own; however, it is possible for bone spurs in the elbow to irritate the bursa, leading to bursitis. Osteotomy may be done alone or with a drainage or bursectomy procedure.
After surgery, patients may be told to wear a sling to keep their arm bent at 90 degrees while healing. Potential complications of surgery include trouble with skin healing at the incision site and tenderness.
Physical Therapy
After nonsurgical or surgical treatment, when elbow bursitis symptoms have abated, a doctor may recommend supervised physical therapy or assign stretches and exercises. Stretching and strengthening activities can help restore normal range of motion and muscle tone to the arm.
It is important to wait until all pain and swelling around the elbow is gone before resuming activities that involve the elbow. Returning to activities that cause friction or stress on the bursa before it is healed will likely cause bursitis symptoms to flare up again.
Physicians who treat elbow bursitis include but are not limited to primary care physicians, physiatrists, sports medicine physicians, and orthopedic surgeons.
Read more about the the different doctors that treat bursitis, an arthritic condition, in Arthritis Treatment Specialists
- 1 Cooper C, Chapurlat R, Al-Daghri N, et al. Safety of Oral Non-Selective Non-Steroidal Anti-Inflammatory Drugs in Osteoarthritis: What Does the Literature Say? Drugs Aging. 2019;36(Suppl 1):15–24. doi:10.1007/s40266-019-00660-1.
- 2 Zimmermann B 3rd, Mikolich DJ, Ho G Jr. Septic bursitis. Semin Arthritis Rheum 1995;24:391-410. As cited in Reilly D, Kamineni S. Olecranon bursitis. J Shoulder Elbow Surg. 2016 Jan;25(1):158-67. doi: 10.1016/j.jse.2015.08.032. Epub 2015 Nov 11. Review. PubMed PMID: 26577126.
- 3 Weinstein PS, Canoso JJ, Wohlgethan JR, "Long-term follow-up of corticosteroid injection for traumatic olecranon bursitis," Ann Rheum Dis, 1984 Feb;43(1):44-6. PubMed PMID: 6696516; PubMed Central PMCID: PMC1001216.
- 4 Brinks A, Koes BW, Volkers AC, Verhaar JA, Bierma-Zeinstra SM, "Adverse effects of extra-articular corticosteroid injections: a systematic review," BMC Musculoskelet Disord, 2010 Sep 13;11:206. Review. PubMed PMID: 20836867; PubMed Central PMCID: PMC2945953.
- 5 Soderquist B, Hedstrom SA. Predisposing factors, bacteriology and antibiotic therapy in 35 cases of septic bursitis. Scand J Infect Dis 1986;18:305-11. As cited in Reilly D, Kamineni S. Olecranon bursitis. J Shoulder Elbow Surg. 2016 Jan;25(1):158-67. doi: 10.1016/j.jse.2015.08.032. Epub 2015 Nov 11. Review. PubMed PMID: 26577126.
- 6 Barnett J, Bernacki MN, Kainer JL, Smith HN, Zaharoff AM, Subramanian SK. The effects of regenerative injection therapy compared to corticosteroids for the treatment of lateral Epicondylitis: a systematic review and meta-analysis. Arch Physiother. 2019;9:12. Published 2019 Nov 13. doi:10.1186/s40945-019-0063-6
- 7 Taylor SA, Hannafin JA. Evaluation and management of elbow tendinopathy. Sports Health. 2012;4(5):384–393. doi:10.1177/1941738112454651
- 8 Blackwell JR, Hay BA, Bolt AM, Hay SM. Olecranon bursitis: a systematic overview. Shoulder Elbow 2014;6:182-90. http://dx.doi. org/10.1177/1758573214532787.
- 9 Raddatz DA, Hoffman GS, Franck WA. Septic bursitis: presentation, treatment and prognosis. J Rheumatol 1987; 14: 1160–1163. As cited in Blackwell JR, Hay BA, Bolt AM, Hay SM. Olecranon bursitis: a systematic overview. Shoulder Elbow. 2014;6(3):182–190. doi:10.1177/1758573214532787