Inflammation in the spine and sacroiliac (SI) joints is caused by a type of chronic, immune-mediated arthritis called ankylosing spondylitis. The condition causes low back pain, spinal rigidity, postural abnormalities, and hip and buttock pain.1Wenker KJ, Quint JM. Ankylosing Spondylitis. [Updated 2023 Apr 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470173/
Arthritis of peripheral joints, such as hips, shoulders, fingers, and toes, also occurs in approximately one-third of cases.1Wenker KJ, Quint JM. Ankylosing Spondylitis. [Updated 2023 Apr 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470173/
The global prevalence of ankylosing spondylitis is less than 2 percent.2Dean LE, Jones GT, MacDonald AG, Downham C, Sturrock RD, Macfarlane GJ. Global prevalence of ankylosing spondylitis. Rheumatology. 2013;53(4):650-657. doi: 10.1093/rheumatology/ket387
In This Article:
The Immune System’s Role in Spinal Inflammation
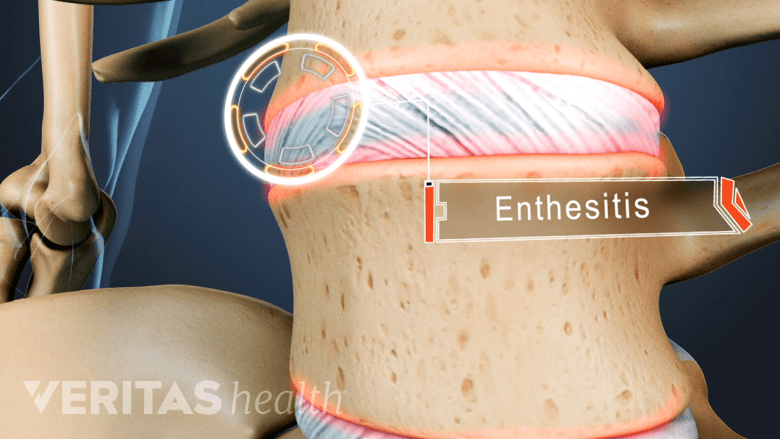
Ankylosing spondylitis mainly affects the entheses, where ligaments attach to bone.
Ankylosing spondylitis primarily affects the entheses – the regions where ligaments, tendons, and joint capsules insert into bone. Over time, chronic inflammation of the entheses (enthesitis) triggers abnormal bone formation, resulting in gradual fusion of the spinal vertebrae, facet joints, and sacroiliac joints. This gradual ossification of the spine leads to loss of flexibility and mobility.3Zhu W, He X, Cheng K, et al. Ankylosing spondylitis: etiology, pathogenesis, and Treatments. Bone Research. 2019;7(1):1-16. doi: 10.1038/s41413-019-0057-8,4Mathew AJ, Østergaard M. Magnetic Resonance Imaging of Enthesitis in Spondyloarthritis, Including Psoriatic Arthritis-Status and Recent Advances. Front Med (Lausanne). 2020;7:296. Published 2020 Jun 30. doi:10.3389/fmed.2020.00296
1. The immune system is triggered
Ankylosing spondylitis is an autoimmune disease, meaning the immune system attacks the body's own tissues.3Zhu W, He X, Cheng K, et al. Ankylosing spondylitis: etiology, pathogenesis, and Treatments. Bone Research. 2019;7(1):1-16. doi: 10.1038/s41413-019-0057-8
Individuals with ankylosing spondylitis have alterations in specific immune cells (T-cells), which make these cells produce more proinflammatory proteins, including1Wenker KJ, Quint JM. Ankylosing Spondylitis. [Updated 2023 Apr 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470173/,3Zhu W, He X, Cheng K, et al. Ankylosing spondylitis: etiology, pathogenesis, and Treatments. Bone Research. 2019;7(1):1-16. doi: 10.1038/s41413-019-0057-8,5Garcia-Montoya L, Gul H, Emery P. Recent advances in ankylosing spondylitis: understanding the disease and management. F1000Res. 2018;7:F1000 Faculty Rev-1512. Published 2018 Sep 21. doi:10.12688/f1000research.14956.1:
- Tumor necrosis factor- α (TNF-α)
- Transforming growth factor-β (TGF-β)
- Interleukin (IL) 23 and IL-17
These proinflammatory proteins stimulate inflammation, cartilage breakdown, and bone erosion in the joints affected by ankylosing spondylitis.5Garcia-Montoya L, Gul H, Emery P. Recent advances in ankylosing spondylitis: understanding the disease and management. F1000Res. 2018;7:F1000 Faculty Rev-1512. Published 2018 Sep 21. doi:10.12688/f1000research.14956.1
2. Enthesitis occurs at different sites in the spine
The inflammatory processes cause repetitive microtraumas at the enthesis, which triggers an inflammatory response in the adjoining tissues, such as fibrocartilage, bursae, synovium, and trabecular bone (the spongy inner bone layer).4Mathew AJ, Østergaard M. Magnetic Resonance Imaging of Enthesitis in Spondyloarthritis, Including Psoriatic Arthritis-Status and Recent Advances. Front Med (Lausanne). 2020;7:296. Published 2020 Jun 30. doi:10.3389/fmed.2020.00296,6Alvarez A, Tiu TK. Enthesopathies. [Updated 2023 Jun 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559030/
In ankylosing spondylitis, inflammation typically begins in the SI joints, but as the disease progresses, the entheses of the facet joints, outer ring of the intervertebral discs, and peripheral joints are affected.6Alvarez A, Tiu TK. Enthesopathies. [Updated 2023 Jun 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559030/
3. Spinal and sacroiliac joint fusion take place
Over time, the inflamed entheses around the SI joints induce changes such as swelling, tissue damage, and bone erosion. The body responds to this inflammation by growing new bone tissue, called enthesophytes, through a process known as calcification.6Alvarez A, Tiu TK. Enthesopathies. [Updated 2023 Jun 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559030/
As the cycle of inflammation, healing, and enthesophyte growth continues, the SI joints can eventually fuse together leading to limited mobility of the lower back or chronic pain.7Wilson DJ, Marcelo de Abreu. Spine Degeneration and Inflammation. IDKD Springer series. Published online January 1, 2021:197-213. doi: 10.1007/978-3-030-71281-5_14,8Dwan K. Understanding Bony Ankylosis: Causes, Symptoms, and Treatment. Rheumatology: Current Research. 2023;13(1):1-2. doi: 10.35248/2161-1146.23.13.331
Progression of ankylosing spondylitis leads to the involvement of the facet joints and intervertebral discs, and the same cycle of inflammation and new bone growth occurs and leads to the fusion of the spinal segments. This process results in reduced function and loss of normal structure in the spine.7Wilson DJ, Marcelo de Abreu. Spine Degeneration and Inflammation. IDKD Springer series. Published online January 1, 2021:197-213. doi: 10.1007/978-3-030-71281-5_14,8Dwan K. Understanding Bony Ankylosis: Causes, Symptoms, and Treatment. Rheumatology: Current Research. 2023;13(1):1-2. doi: 10.35248/2161-1146.23.13.331
See Development and Progression of Ankylosing Spondylitis
Additionally, the vertebral bodies undergo erosion and inflammation, leading to a transformation in their shape, making them more square-like. New bone tissue, called syndesmophytes, grows over these square-shaped vertebrae, resulting in complete fusion of the vertebrae (ankylosis) and spinal immobility.7Wilson DJ, Marcelo de Abreu. Spine Degeneration and Inflammation. IDKD Springer series. Published online January 1, 2021:197-213. doi: 10.1007/978-3-030-71281-5_14,8Dwan K. Understanding Bony Ankylosis: Causes, Symptoms, and Treatment. Rheumatology: Current Research. 2023;13(1):1-2. doi: 10.35248/2161-1146.23.13.331
Hallmark Symptoms and Signs of Ankylosing Spondylitis
Ankylosing spondylitis causes pain in the lower back, hip, and buttocks.
Several areas of the low back, pelvis, and thigh are affected in ankylosing spondylitis. The symptoms typically appear before the age of 45 and include some combination of1Wenker KJ, Quint JM. Ankylosing Spondylitis. [Updated 2023 Apr 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470173/,9Akhondi H, Varacallo M. Rheumatoid Arthritis and Ankylosing Spondylitis. [Updated 2022 Sep 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532288/:
- Chronic low back pain that typically improves with movement and exercise
- Spinal stiffness that is generally worse in the mornings
- Hip pain that typically goes into the thigh
- Buttock pain that typically alternates but is sometimes one-sided
- SI joint pain that usually occurs when sitting or standing
Ankylosing spondylitis can also involve the peripheral joints and cause pain in the shoulders, ankles, and knees; neck pain and stiffness; and inflammation and swelling of the fingers and toes (dactylitis), leading to the appearance of sausage digits.1Wenker KJ, Quint JM. Ankylosing Spondylitis. [Updated 2023 Apr 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470173/
Co-Occurring Conditions with Ankylosing Spondylitis
Certain inflammatory conditions with similar characteristics co-occur with ankylosing spondylitis, including1Wenker KJ, Quint JM. Ankylosing Spondylitis. [Updated 2023 Apr 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470173/,10Stolwijk C, van Tubergen A, Castillo-Ortiz JD, Boonen A. Prevalence of extra-articular manifestations in patients with ankylosing spondylitis: a systematic review and meta-analysis. Annals of the Rheumatic Diseases. 2013;74(1):65-73. doi: 10.1136/annrheumdis-2013-203582:
- Inflammatory bowel disease: inflammation of the gastrointestinal tract, which affects up to 50% of people with ankylosing spondylitis
- Acute anterior uveitis: inflammation of the uveal tract in the eyes, which affects 25% to 35% of people with ankylosing spondylitis
- Psoriasis: an inflammatory condition affecting the skin, which affects 10% of people with ankylosing spondylitis
These conditions share genetic susceptibility factors and alterations in immune functions with ankylosing spondylitis.1Wenker KJ, Quint JM. Ankylosing Spondylitis. [Updated 2023 Apr 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470173/,10Stolwijk C, van Tubergen A, Castillo-Ortiz JD, Boonen A. Prevalence of extra-articular manifestations in patients with ankylosing spondylitis: a systematic review and meta-analysis. Annals of the Rheumatic Diseases. 2013;74(1):65-73. doi: 10.1136/annrheumdis-2013-203582
The Course of Ankylosing Spondylitis
Ankylosing spondylitis cannot be cured, but managing inflammation is a critical factor in limiting the course and severity of the disease.11Sen R, Goyal A, Hurley JA. Seronegative Spondyloarthropathy. [Updated 2023 Jul 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459356/
As the condition advances, chronic inflammatory processes in the upper back (thoracic spine) affect the costotransverse and costovertebral joints where the ribs attach to the spine, affecting posture and restricting lung capacity.1Wenker KJ, Quint JM. Ankylosing Spondylitis. [Updated 2023 Apr 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470173/,12Waxenbaum JA, Reddy V, Futterman B. Anatomy, Back, Thoracic Vertebrae. [Updated 2023 Aug 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459153/ Neck pain develops in the later stages as the cervical spine becomes involved.13Xiong Y, Cai M, Xu Y, et al. Joint together: The etiology and pathogenesis of ankylosing spondylitis. Front Immunol. 2022;13:996103. Published 2022 Oct 17. doi:10.3389/fimmu.2022.996103
Severe disability is uncommon, and most people with ankylosing spondylitis remain able to work and participate in daily activities.1Wenker KJ, Quint JM. Ankylosing Spondylitis. [Updated 2023 Apr 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470173/ However, the presence of one or more co-occurring inflammatory conditions (eg, psoriasis) is associated with poor prognosis and negatively influences quality of life.10Stolwijk C, van Tubergen A, Castillo-Ortiz JD, Boonen A. Prevalence of extra-articular manifestations in patients with ankylosing spondylitis: a systematic review and meta-analysis. Annals of the Rheumatic Diseases. 2013;74(1):65-73. doi: 10.1136/annrheumdis-2013-203582
See Progression of Ankylosing Spondylitis in the Spine
Impact of Ankylosing Spondylitis on Daily Life and Activities
Quality of life doesn't necessarily decline significantly for every individual with ankylosing spondylitis.14Rosenbaum JT, Pisenti L, Park Y, Howard RA. Insight into the Quality of Life of Patients with Ankylosing Spondylitis: Real-World Data from a US-Based Life Impact Survey. Rheumatol Ther. 2019;6(3):353-367. doi:10.1007/s40744-019-0160-8
The most common limitations include a reduced ability to keep physically active and increased discomfort when sitting for long periods of time during travel or work.14Rosenbaum JT, Pisenti L, Park Y, Howard RA. Insight into the Quality of Life of Patients with Ankylosing Spondylitis: Real-World Data from a US-Based Life Impact Survey. Rheumatol Ther. 2019;6(3):353-367. doi:10.1007/s40744-019-0160-8
When Ankylosing Spondylitis Is Serious
In the advanced stages, ankylosing spondylitis is characterized by postural abnormalities and severe spinal damage, including:
- Cauda equina syndrome: a medical emergency involving damage to the cauda equina nerve roots that causes problems with bladder and bowel control and impotence.15Rider LS, Marra EM. Cauda Equina and Conus Medullaris Syndromes. [Updated 2023 Aug 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537200/
- Spondylodiscitis: an infection that affects the vertebrae, spinal discs, and adjacent structures.16Kaynar R, Sarı H, Uludağ M, Atarod N. FRI0231 Spondylodiscitis in Patients with Ankylosing Spondylitis: A Retrospective Study of 16 Cases. Annals of the Rheumatic Diseases. 2015;74(Suppl 2):508.2-508. doi:10.1136/annrheumdis-2015-eular.1341,17Homagk L, Marmelstein D, Homagk N, Hofmann GO. SponDT (Spondylodiscitis Diagnosis and Treatment): spondylodiscitis scoring system. Journal of Orthopaedic Surgery and Research. 2019;14(1). doi: 10.1186/s13018-019-1134-9
- Hunched back: also referred to as hyperkyphosis, hunched back is characterized by an excessive forward curvature of the upper spine, leading to an exaggerated rounding of the upper back caused by abnormal bone growth in the advanced stages of ankylosing spondylitis.18Lam JC, Mukhdomi T. Kyphosis. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK558945/
- Fractures: both vertebral and non-vertebral fractures occur due to the fragility of the bones caused by low bone mineral density and spinal rigidity.19Pray C, Feroz NI, Nigil Haroon N. Bone Mineral Density and Fracture Risk in Ankylosing Spondylitis: A Meta-Analysis. Calcif Tissue Int. 2017;101(2):182-192. doi:10.1007/s00223-017-0274-3
- Bamboo spine: a hallmark late-stage finding in ankylosing spondylitis caused by fusion of the vertebrae and is associated with progressive back stiffness.1Wenker KJ, Quint JM. Ankylosing Spondylitis. [Updated 2023 Apr 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470173/
Cauda equina syndrome requires immediate medical treatment to prevent permanent nerve damage, such as bladder dysfunction and paralysis.15Rider LS, Marra EM. Cauda Equina and Conus Medullaris Syndromes. [Updated 2023 Aug 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537200/ Spondylodiscitis and spinal fractures also require medical intervention to prevent complications, but they are not usually considered emergencies.16Kaynar R, Sarı H, Uludağ M, Atarod N. FRI0231 Spondylodiscitis in Patients with Ankylosing Spondylitis: A Retrospective Study of 16 Cases. Annals of the Rheumatic Diseases. 2015;74(Suppl 2):508.2-508. doi:10.1136/annrheumdis-2015-eular.1341,17Homagk L, Marmelstein D, Homagk N, Hofmann GO. SponDT (Spondylodiscitis Diagnosis and Treatment): spondylodiscitis scoring system. Journal of Orthopaedic Surgery and Research. 2019;14(1). doi: 10.1186/s13018-019-1134-9,19Pray C, Feroz NI, Nigil Haroon N. Bone Mineral Density and Fracture Risk in Ankylosing Spondylitis: A Meta-Analysis. Calcif Tissue Int. 2017;101(2):182-192. doi:10.1007/s00223-017-0274-3
Complications in the Peripheral Joints and Organs
Non-spinal complications of ankylosing spondylitis occur in the peripheral joints and organs that are affected by chronic inflammation, including1Wenker KJ, Quint JM. Ankylosing Spondylitis. [Updated 2023 Apr 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470173/,20Zhao SS, Robertson S, Reich T, Harrison NL, Moots RJ, son NJ. Prevalence and impact of comorbidities in axial spondyloarthritis: systematic review and meta-analysis. Rheumatology (Oxford). 2020;59(Suppl4):iv47-iv57. doi:10.1093/rheumatology/keaa246,21Eriksson JK, Jacobsson L, Bengtsson K, Askling J. Is ankylosing spondylitis a risk factor for cardiovascular disease, and how do these risks compare with those in rheumatoid arthritis?. Ann Rheum Dis. 2017;76(2):364-370. doi:10.1136/annrheumdis-2016-209315:
- Heart disease, such as high blood pressure, heart failure, aortic regurgitation, stroke, and acute coronary syndrome
- Respiratory conditions, such as pulmonary fibrosis and restrictive pulmonary disease, which is also caused and/or or worsened by reduced chest wall expansion
Additionally, chronic pain and disability lead to fatigue, sleep disturbances, and mood disorders such as depression in some cases.20Zhao SS, Robertson S, Reich T, Harrison NL, Moots RJ, son NJ. Prevalence and impact of comorbidities in axial spondyloarthritis: systematic review and meta-analysis. Rheumatology (Oxford). 2020;59(Suppl4):iv47-iv57. doi:10.1093/rheumatology/keaa246
Specialists Who Treat Ankylosing Spondylitis
A rheumatologist or spine specialist usually diagnoses, treats, and monitors patients with ankylosing spondylitis.1Wenker KJ, Quint JM. Ankylosing Spondylitis. [Updated 2023 Apr 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470173/
Consultation with a physical therapist is also beneficial for individualized exercise plans to improve posture, spine mobility, and strength.1Wenker KJ, Quint JM. Ankylosing Spondylitis. [Updated 2023 Apr 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470173/
- 1 Wenker KJ, Quint JM. Ankylosing Spondylitis. [Updated 2023 Apr 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470173/
- 2 Dean LE, Jones GT, MacDonald AG, Downham C, Sturrock RD, Macfarlane GJ. Global prevalence of ankylosing spondylitis. Rheumatology. 2013;53(4):650-657. doi: 10.1093/rheumatology/ket387
- 3 Zhu W, He X, Cheng K, et al. Ankylosing spondylitis: etiology, pathogenesis, and Treatments. Bone Research. 2019;7(1):1-16. doi: 10.1038/s41413-019-0057-8
- 4 Mathew AJ, Østergaard M. Magnetic Resonance Imaging of Enthesitis in Spondyloarthritis, Including Psoriatic Arthritis-Status and Recent Advances. Front Med (Lausanne). 2020;7:296. Published 2020 Jun 30. doi:10.3389/fmed.2020.00296
- 5 Garcia-Montoya L, Gul H, Emery P. Recent advances in ankylosing spondylitis: understanding the disease and management. F1000Res. 2018;7:F1000 Faculty Rev-1512. Published 2018 Sep 21. doi:10.12688/f1000research.14956.1
- 6 Alvarez A, Tiu TK. Enthesopathies. [Updated 2023 Jun 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559030/
- 7 Wilson DJ, Marcelo de Abreu. Spine Degeneration and Inflammation. IDKD Springer series. Published online January 1, 2021:197-213. doi: 10.1007/978-3-030-71281-5_14
- 8 Dwan K. Understanding Bony Ankylosis: Causes, Symptoms, and Treatment. Rheumatology: Current Research. 2023;13(1):1-2. doi: 10.35248/2161-1146.23.13.331
- 9 Akhondi H, Varacallo M. Rheumatoid Arthritis and Ankylosing Spondylitis. [Updated 2022 Sep 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532288/
- 10 Stolwijk C, van Tubergen A, Castillo-Ortiz JD, Boonen A. Prevalence of extra-articular manifestations in patients with ankylosing spondylitis: a systematic review and meta-analysis. Annals of the Rheumatic Diseases. 2013;74(1):65-73. doi: 10.1136/annrheumdis-2013-203582
- 11 Sen R, Goyal A, Hurley JA. Seronegative Spondyloarthropathy. [Updated 2023 Jul 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459356/
- 12 Waxenbaum JA, Reddy V, Futterman B. Anatomy, Back, Thoracic Vertebrae. [Updated 2023 Aug 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459153/
- 13 Xiong Y, Cai M, Xu Y, et al. Joint together: The etiology and pathogenesis of ankylosing spondylitis. Front Immunol. 2022;13:996103. Published 2022 Oct 17. doi:10.3389/fimmu.2022.996103
- 14 Rosenbaum JT, Pisenti L, Park Y, Howard RA. Insight into the Quality of Life of Patients with Ankylosing Spondylitis: Real-World Data from a US-Based Life Impact Survey. Rheumatol Ther. 2019;6(3):353-367. doi:10.1007/s40744-019-0160-8
- 15 Rider LS, Marra EM. Cauda Equina and Conus Medullaris Syndromes. [Updated 2023 Aug 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537200/
- 16 Kaynar R, Sarı H, Uludağ M, Atarod N. FRI0231 Spondylodiscitis in Patients with Ankylosing Spondylitis: A Retrospective Study of 16 Cases. Annals of the Rheumatic Diseases. 2015;74(Suppl 2):508.2-508. doi:10.1136/annrheumdis-2015-eular.1341
- 17 Homagk L, Marmelstein D, Homagk N, Hofmann GO. SponDT (Spondylodiscitis Diagnosis and Treatment): spondylodiscitis scoring system. Journal of Orthopaedic Surgery and Research. 2019;14(1). doi: 10.1186/s13018-019-1134-9
- 18 Lam JC, Mukhdomi T. Kyphosis. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK558945/
- 19 Pray C, Feroz NI, Nigil Haroon N. Bone Mineral Density and Fracture Risk in Ankylosing Spondylitis: A Meta-Analysis. Calcif Tissue Int. 2017;101(2):182-192. doi:10.1007/s00223-017-0274-3
- 20 Zhao SS, Robertson S, Reich T, Harrison NL, Moots RJ, son NJ. Prevalence and impact of comorbidities in axial spondyloarthritis: systematic review and meta-analysis. Rheumatology (Oxford). 2020;59(Suppl4):iv47-iv57. doi:10.1093/rheumatology/keaa246
- 21 Eriksson JK, Jacobsson L, Bengtsson K, Askling J. Is ankylosing spondylitis a risk factor for cardiovascular disease, and how do these risks compare with those in rheumatoid arthritis?. Ann Rheum Dis. 2017;76(2):364-370. doi:10.1136/annrheumdis-2016-209315

