If not properly treated, a case of bursitis can turn into chronic bursitis, flaring up on and off for several weeks, months, or even longer. Bursitis treatment involves strategies to decrease inflammation in the bursa.
Many bursitis treatments can be done at home. However, medical treatments may be necessary if the swelling and pain do not lessen after a week or two of home treatments. Surgery is rarely needed.
Medical treatment is necessary when Septic Bursitis is suspected, because the infection can spread to other points in the body, including the bloodstream—while not common, this condition is life-threatening.
Once bursitis has occurred in a bursa, there is a risk of it coming back. Thankfully, steps can be taken to prevent bursitis from recurring.
In This Article:
- What Is Bursitis?
- Bursitis Treatment and Prevention
Home Treatments for Bursitis
Taking a few simple steps at home may effectively treat non-infectious bursitis. These steps include:
- Resting the joint by avoiding activities that may irritate the bursa, allowing the inflammation time to subside
- Wearing comfortable, supportive, low-heeled shoes if bursitis affects a weight-bearing joint
- Taking non-steroidal anti-inflammatory medications, such as ibuprofen
- Applying a cold compress, which can ease inflammation
A cold compress can be applied 2 to 3 times a day for 10 to 20 minutes. If using ice, wrap it in a towel to avoid injury to the skin.
Medical Treatments for Bursitis
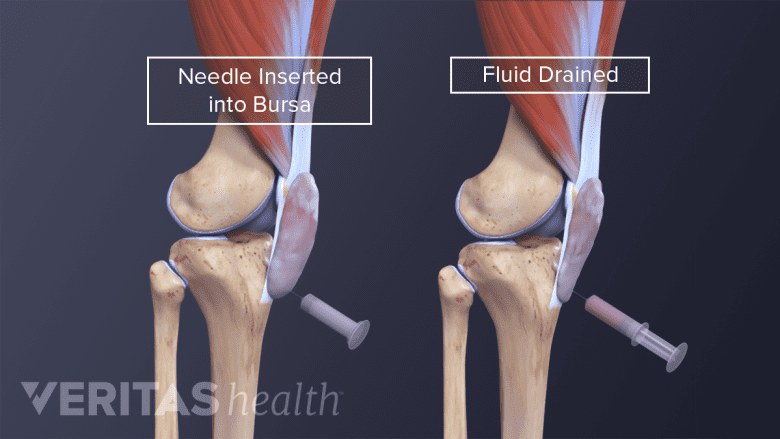
Fluid may be drained from the bursa using a process called needle aspiration.
When home treatments have not eased symptoms, symptoms are severe, or septic bursitis is suspected, then medical treatment is advised. Depending on the circumstances, a doctor may recommend continued home treatment as well as:
- Physical therapy to strengthen and stretch the tissues around the affected bursa
- Orthotics to improve body mechanics and take stress of the bursa
- A bursal aspiration to remove excess fluid from the bursa
- A cortisone injection to quickly reduce inflammation (typically done along with an aspiration)
- Therapeutic ultrasound to stimulate blood flow and healing1Ma, CB. Bursitis of the heel. MedlinePlus, US National Library of Medicine. Updated August 15, 2018. Accessed January 25, 2021. https://medlineplus.gov/ency/article/001073.htm
- Antibiotics for cases of septic bursitis
Not all of the above treatments are appropriate for all types of bursitis. For example, physical therapy may be appropriate if the inflamed bursa is located under a tight tendon or muscle, but it may not be helpful if the bursa is located just below the skin.
In addition, doctors do not agree on all treatment approaches. For example, while some doctors may recommend cortisone injections for prepatellar bursitis, others discourage this approach, citing research that suggests cortisone injections are not an effective treatment.2Khodaee M. Common Superficial Bursitis. Am Fam Physician. 2017 Feb 15;95(4):224-231. PMID: 28290630.
All medical treatments carry potential side effects. Talk to your doctor to find out about the associated risks.
Surgery for Bursitis: Bursectomy
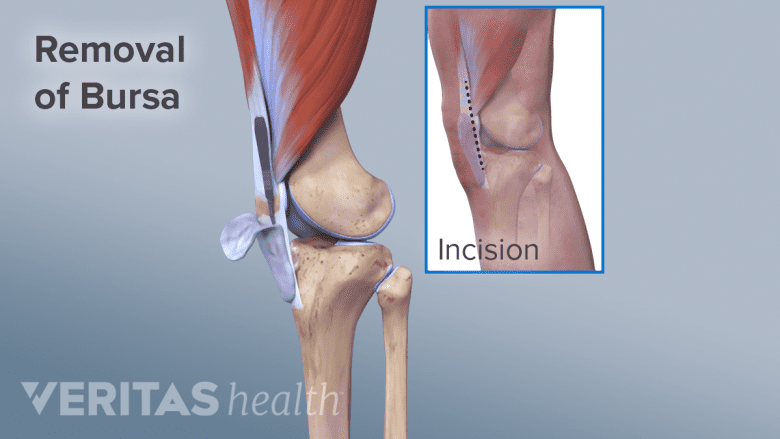
In the process of a bursectomy, the inflamed bursa is surgically removed.
If bursitis is chronic and difficult to treat, a doctor may suggest a surgery called a bursectomy. During this surgery, the inflamed bursa is removed.
A bursectomy may be done along with other surgical procedures. For example, a surgeon may remove an inflamed bursa from the back of the heel as well as the bone spurs that contributed to the bursa’s irritation.
After surgery, a bursa may grow back. The hope is that the new bursa will be less prone to inflammation.
Sclerotherapy
A newer and less proven approach to eliminating the troublesome bursa is sclerotherapy. This treatment involves shrinking and killing the bursal tissue. This procedure is done by injecting a chemical irritant into the inflamed bursa,3Parker CH, Leggit JC. Novel Treatment of Prepatellar Bursitis. Mil Med. 2018 Nov 01;183(11-12):e768-e770. [PubMed] [Reference list],4Rishor-Olney CR, Pozun A. Prepatellar Bursitis. [Updated 2020 Dec 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557508/ causing the bursal tissue to die.
Sclerotherapy treatment is much less common than bursectomy. It may not always be an available or appropriate substitute for bursectomy.
Bursitis Prevention Strategies
People who have a history of bursitis may want to take steps to lower the risk of recurrence. One or more of the following prevention strategies may be recommended:
- Take regular breaks from repetitive motions that might irritate bursae
- Avoid certain positions that irritate the affected bursa, such as kneeling or leaning on the elbows
- Wear cushioned knee or elbow pads to help protect a bursa when kneeling or leaning on the elbows is unavoidable
- Support good body mechanics by wearing comfortable, supportive, low-heeled shoes and/or an orthotic, such as a shoe insert or knee brace
- Exercise to strengthen and stretch the tissues around the affected joint
- Treat underlying medical conditions, such as rheumatoid arthritis, that may be associated with bursitis
Which strategies may effectively prevent bursitis will depend on many factors, especially which bursa is affected. For example, avoiding kneeling or wearing knee pads can decrease the risk of triggering bursitis in the prepatellar bursa, which is located between the kneecap and the skin. However, those strategies would not work to prevent bursitis in the knee’s pes anserine bursa, which is located between the shin’s tibia bone and the hamstring muscle tendons.
- 1 Ma, CB. Bursitis of the heel. MedlinePlus, US National Library of Medicine. Updated August 15, 2018. Accessed January 25, 2021. https://medlineplus.gov/ency/article/001073.htm
- 2 Khodaee M. Common Superficial Bursitis. Am Fam Physician. 2017 Feb 15;95(4):224-231. PMID: 28290630.
- 3 Parker CH, Leggit JC. Novel Treatment of Prepatellar Bursitis. Mil Med. 2018 Nov 01;183(11-12):e768-e770. [PubMed] [Reference list]
- 4 Rishor-Olney CR, Pozun A. Prepatellar Bursitis. [Updated 2020 Dec 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557508/

