When a bursa is infected, it is called septic bursitis. Septic bursitis typically affects bursae located at the knee and elbow joints. Unlike aseptic (non-infectious) bursitis, septic bursitis is a potentially serious medical condition and prompt medical attention is advisable.
See What Is a Bursa?
In This Article:
- Septic Bursitis
- Septic Bursitis Treatment
Symptoms of Bursitis
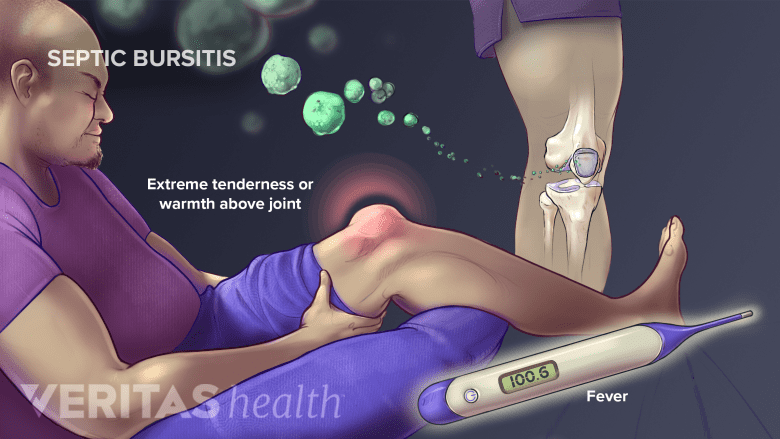
If a bursa is infected, a person will likely experience the typical symptoms of bursitis, particularly joint swelling and tenderness, as well as:
- Skin that is warm to the touch. The temperature of the skin over the inflamed bursa may be warmer than elsewhere.1Smith DL, McAfee JH, Lucas LM, Kumar KL, Romney DM. "Septic and nonseptic olecranon bursitis. Utility of the surface temperature probe in the early differentiation of septic and nonseptic cases," (Abstract only) Arch Intern Med, 1989;149(7):1581-1585. PMID 2742432.
- Skin redness. The skin over the inflamed bursa may appear red.
- Fever. A high fever and/or chills (in addition to other bursitis symptoms) can be a sign of septic bursitis. One study reported that up to 77% of people with septic bursitis had a fever.2García-Porrúa C, González-Gay MA, Ibañez D, García-País MJ. J Rheumatol. 1999 Mar; 26(3):663-7. As cited in Blackwell JR, Hay BA, Bolt AM, Hay SM. Olecranon bursitis: a systematic overview. Shoulder Elbow. 2014;6(3):182–190. doi:10.1177/1758573214532787.
- A general feeling of being sick. A person may feel unwell or “off.”
These symptoms may appear even if the bursitis is aseptic (non-infectious). For this reason, distinguishing between aseptic bursitis and septic bursitis can be challenging.
Read more about Bursitis Symptoms
Consult with a doctor if there is any doubt as to whether a bursa may be infected.
Bursae and Septic Bursitis
Bursae are small, thin, slippery sacs filled with lubricating fluid. They are located near joints throughout the body and help decrease friction between bone and soft tissues. For example, at the heel, the retrocalcaneal bursa serves as a lubricating cushion between the foot’s calcaneal bone and the Achilles tendon.
Septic bursitis is most likely to occur in bursae that lie just below the skin, such as the prepatellar bursa at the kneecap and the olecranon bursa at the tip of the elbow. These bursae are called superficial bursae.
- See the symptoms and treatments for:
How Microorganisms Infect Bursae
A bursa can become infected when bacteria or other microorganisms in the body enter the bursal sac and multiply. The microorganism may come from:
- Outside the body. Microorganisms can enter the bursa through a cut, scrape, puncture, bug bite, or other means. Sometimes the infection occurs without an obvious entry point on the skin.
People who may be more susceptible to get septic bursitis this way are those who spend a lot of time on their knees and elbows, such as plumbers, carpenters, roofers, clergy, and athletes. 3Truong J, Ashurst JV. Septic Bursitis. 2019 Jan;. Review. PubMed PMID: 29262131. - Inside the body. While less common, it is possible for infectious microorganism elsewhere in the body to enter the bursa. For example, it is possible for the bacteria causing septic arthritis or tuberculosis to infect a bursa.4Lormeau C, Cormier G, Sigaux J, Arvieux C, Semerano L. Management of septic bursitis . Joint Bone Spine. 2019 Oct;86(5):583-588. doi: 10.1016/j.jbspin.2018.10.006. Epub 2018 Oct 26. PubMed PMID: 31615686.
In some cases, a needle puncture from an aspiration (to drain the swollen bursa) or a corticosteroid injection to treat aseptic bursitis can trigger septic bursitis.5Teoh KH, Jones SA, Gurunaidu S, Pritchard MG. Methicillin-resistant Staphylococcus aureus infection of the subacromial bursa: an unusual complication following subacromial corticosteroid injection (a report of two cases). Shoulder Elb 2015;7:182–6. As cited in Lormeau C, Cormier G, Sigaux J, Arvieux C, Semerano L. Management of septic bursitis. Joint Bone Spine. 2019 Oct;86(5):583-588. doi: 10.1016/j.jbspin.2018.10.006. Epub 2018 Oct 26. PubMed PMID: 31615686.,6Novatnack ES, Protzman NM, Weiss CB. Primary septic greater trochanteric bursitis. J Glob Infect Dis 2015;7:93–4. As cited in Lormeau C, Cormier G, Sigaux J, Arvieux C, Semerano L. Management of septic bursitis. Joint Bone Spine. 2019 Oct;86(5):583-588. doi: 10.1016/j.jbspin.2018.10.006. Epub 2018 Oct 26. PubMed PMID: 31615686.
Medical Conditions Associated with Septic Bursitis
People who have certain forms of inflammatory arthritis or weakened immune systems (including due to medications) of are more likely to develop septic bursitis. For example, the following can increase the risk for septic bursitis3Truong J, Ashurst JV. Septic Bursitis. 2019 Jan;. Review. PubMed PMID: 29262131.,7Reilly D, Kamineni S. Olecranon bursitis. J Shoulder Elbow Surg. 2016 Jan;25(1):158-67. doi: 10.1016/j.jse.2015.08.032. Epub 2015 Nov 11. Review. PubMed PMID: 26577126.,8Roschmann RA, Bell CL. Septic bursitis in immunocompromised patients. Am J Med 1987; 83: 661–665.:
- Diabetes, particularly if it is not well controlled
- Chronic obstructive pulmonary disease (COPD)
- Alcoholism
- Inflammatory arthritis, including rheumatoid arthritis
- Crystal deposit arthritis, including gout and pseudogout (also knowns as calcium pyrophosphate deposition, or CPPD)
- Medications that suppress the immune system, such as corticosteroids
People who have significant immunosuppression tend to be more challenging to treat and take longer to heal.7Reilly D, Kamineni S. Olecranon bursitis. J Shoulder Elbow Surg. 2016 Jan;25(1):158-67. doi: 10.1016/j.jse.2015.08.032. Epub 2015 Nov 11. Review. PubMed PMID: 26577126.
Diagnosing Septic Bursitis

Arthrosis, or needle aspiration, may be used to remove joint fluid.
A doctor or other medical professional will begin the diagnostic process by taking the patient’s history and conducting a physical evaluation. He or she may also remove fluid from the affected bursa using a needle and syringe (needle aspiration).
See The Joint Aspiration Procedure
Removing fluid from the bursa can relieve pressure and make the patient more comfortable. It also provides a fluid sample that can be analyzed for infection using lab tests,9Khodaee M. Common Superficial Bursitis. Am Fam Physician. 2017 Feb 15;95(4):224-231. PubMed PMID: 28290630. such as a:
- Blood cell count. A high number of white blood cells in the bursa’s synovial fluid indicates an infection.
- Glucose levels test. Glucose levels that are significantly lower than normal may indicate infection.
- Crystal analysis. The presence of crystals in the bursal fluid indicates gout or pseudogout.
- Gram stain. A lab test called a Gram stain is used to determine if certain infectious bacteria are present.
It is possible for one or more of these tests to come back negative even when the bursa is infected.3Truong J, Ashurst JV. Septic Bursitis. 2019 Jan;. Review. PubMed PMID: 29262131.,7Reilly D, Kamineni S. Olecranon bursitis. J Shoulder Elbow Surg. 2016 Jan;25(1):158-67. doi: 10.1016/j.jse.2015.08.032. Epub 2015 Nov 11. Review. PubMed PMID: 26577126.,10Gowe I, Parsons C, Best M, Parsons E, Prechter S, Vickery S. Successful Treatment of Olecranon Bursitis Caused by Trueperella bernardiae: Importance of Environmental Exposure and Pathogen Identification. Case Rep Infect Dis. 2018;2018:5353085. Published 2018 Sep 4. doi:10.1155/2018/5353085 For example, not all problematic bacteria can be identified with a gram stain, so even if the test comes back negative, septic bursitis cannot be completely ruled out.
Additional lab tests on the bursal fluid or patient’s blood may be used to help diagnose or rule out other medical conditions, such as rheumatoid arthritis and gout. These conditions can cause joint pain and swelling and also increase the risk for septic bursitis.
- 1 Smith DL, McAfee JH, Lucas LM, Kumar KL, Romney DM. "Septic and nonseptic olecranon bursitis. Utility of the surface temperature probe in the early differentiation of septic and nonseptic cases," (Abstract only) Arch Intern Med, 1989;149(7):1581-1585. PMID 2742432.
- 2 García-Porrúa C, González-Gay MA, Ibañez D, García-País MJ. J Rheumatol. 1999 Mar; 26(3):663-7. As cited in Blackwell JR, Hay BA, Bolt AM, Hay SM. Olecranon bursitis: a systematic overview. Shoulder Elbow. 2014;6(3):182–190. doi:10.1177/1758573214532787.
- 3 Truong J, Ashurst JV. Septic Bursitis. 2019 Jan;. Review. PubMed PMID: 29262131.
- 4 Lormeau C, Cormier G, Sigaux J, Arvieux C, Semerano L. Management of septic bursitis . Joint Bone Spine. 2019 Oct;86(5):583-588. doi: 10.1016/j.jbspin.2018.10.006. Epub 2018 Oct 26. PubMed PMID: 31615686.
- 5 Teoh KH, Jones SA, Gurunaidu S, Pritchard MG. Methicillin-resistant Staphylococcus aureus infection of the subacromial bursa: an unusual complication following subacromial corticosteroid injection (a report of two cases). Shoulder Elb 2015;7:182–6. As cited in Lormeau C, Cormier G, Sigaux J, Arvieux C, Semerano L. Management of septic bursitis. Joint Bone Spine. 2019 Oct;86(5):583-588. doi: 10.1016/j.jbspin.2018.10.006. Epub 2018 Oct 26. PubMed PMID: 31615686.
- 6 Novatnack ES, Protzman NM, Weiss CB. Primary septic greater trochanteric bursitis. J Glob Infect Dis 2015;7:93–4. As cited in Lormeau C, Cormier G, Sigaux J, Arvieux C, Semerano L. Management of septic bursitis. Joint Bone Spine. 2019 Oct;86(5):583-588. doi: 10.1016/j.jbspin.2018.10.006. Epub 2018 Oct 26. PubMed PMID: 31615686.
- 7 Reilly D, Kamineni S. Olecranon bursitis. J Shoulder Elbow Surg. 2016 Jan;25(1):158-67. doi: 10.1016/j.jse.2015.08.032. Epub 2015 Nov 11. Review. PubMed PMID: 26577126.
- 8 Roschmann RA, Bell CL. Septic bursitis in immunocompromised patients. Am J Med 1987; 83: 661–665.
- 9 Khodaee M. Common Superficial Bursitis. Am Fam Physician. 2017 Feb 15;95(4):224-231. PubMed PMID: 28290630.
- 10 Gowe I, Parsons C, Best M, Parsons E, Prechter S, Vickery S. Successful Treatment of Olecranon Bursitis Caused by Trueperella bernardiae: Importance of Environmental Exposure and Pathogen Identification. Case Rep Infect Dis. 2018;2018:5353085. Published 2018 Sep 4. doi:10.1155/2018/5353085

