When gout causes severe joint pain, it is called a gout attack, a gout flare-up, or acute gout. Pain is typically accompanied by extreme joint tenderness, swelling, warmth, and skin redness. The symptoms may come on suddenly and without warning.
Gout is acute, painful swelling in the joints from uric acid buildup, often in the foot and big toe.
Experts estimate gout will affect 4% of Americans during their lifetimes, and often occurs in men and people over age 60.1Zhu Y, Pandya BJ, Choi HK. Prevalence of gout and hyperuricemia in the US general population: the National Health and Nutrition Examination Survey 2007-2008. Arthritis Rheum 2011;63(10):3136–41. As cited in Sidari A, Hill E. Diagnosis and Treatment of Gout and Pseudogout for Everyday Practice. Prim Care. 2018;45(2):213-236. doi:10.1016/j.pop.2018.02.004 Typically, only one joint is affected at a time, but it is possible to have several joints affected during a gout attack.
In This Article:
- All About Gout - Symptoms, Diagnosis, Treatment
- Gout Symptoms
- Gout Causes and Risk Factors
- Gout Diagnosis
- Gout Treatment
- Gout Prevention
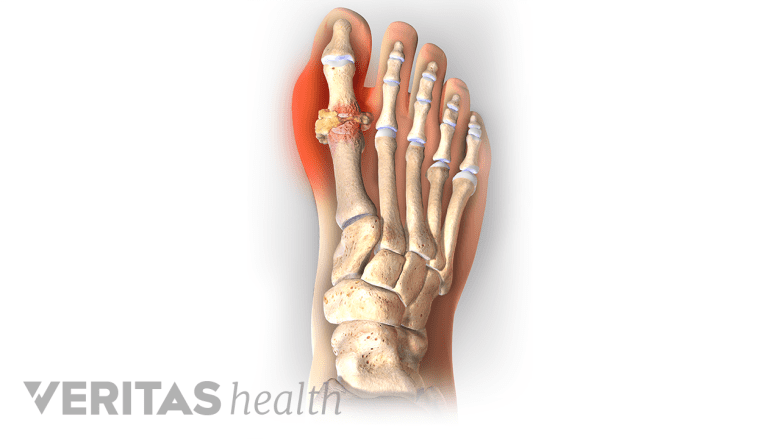
Joints Affected by Gout
Gout can affect any joint, but some joints are more likely to be affected than others. Joints commonly affected include the big toe, the foot’s instep, heel, ankle, and knee.2Sidari A, Hill E. Diagnosis and Treatment of Gout and Pseudogout for Everyday Practice. Prim Care. 2018;45(2):213-236. doi:10.1016/j.pop.2018.02.004 Less often, gout affects the elbow, wrist, fingertips, or spine.2Sidari A, Hill E. Diagnosis and Treatment of Gout and Pseudogout for Everyday Practice. Prim Care. 2018;45(2):213-236. doi:10.1016/j.pop.2018.02.004,3Riddell CM, Elliott M, Cairns, AP. An Unusual "Gouty" Case of Back Pain and Fever. J Rheumatol October 2008 35(10):2076-2077 PMID: 18843766,4Bang SY, Jeong JH, Joo KB, Jun JB, Sung YK. A Case of the Lumbar Spine Involvement and Sacroiliitis in a Patient with Gout. J Korean Rheum Assoc. 2009 Dec;16(4):318-322. https://doi.org/10.4078/jkra.2009.16.4.318,5Mantle B, Gross P, Lopez-Ben R, Alarcón GS. Hip pain as the presenting manifestation of acute gouty sacroiliitis. J Clin Rheumatol. 2001 Apr;7(2):112-4. PubMed PMID: 17039107.,6Konatalapalli RM, Demarco PJ, Jelinek JS, Murphey M, Gibson M, Jennings B, Weinstein A. Gout in the axial skeleton. J Rheumatol. 2009 Mar;36(3):609-13. doi: 10.3899/jrheum.080374. Epub 2009 Feb 4. PubMed PMID: 19208604.,7Klauser AS, Halpern EJ, Strobl S, et al. Gout of hand and wrist: the value of US as compared with DECT. Eur Radiol. 2018;28(10):4174-4181. DOI: 10.1007/s00330-018-5363-9
Differences between men and women
Sex differences play a role in which joints are affected:
- In men, about 85% of gout flare-ups affect joints in the lower extremities. About 50% of first-time gout attacks involve a big toe joint.8Slobodonick A, Toprover M, Pillinger M. Crystal Arthritis. In: Efthimiou P, ed. Absolute Rheumatology Review. Springer Nature Switzerland AG; 2020; chap 15. Accessed September 15, 2020. https://doi.org/10.1007/978-3-030-23022-7_15
- In women, a gout attack is most likely to occur in a knee.10Scott JT, Pollard AC. Uric acid excretion in the relatives of patients with gout. Ann Rheum Dis. 1970 Jul;29(4):397-400. Review. PubMed PMID: 4916770; PubMed Central PMCID: PMC1031324. DOI: 10.1136/ard.29.4.397 In addition, women may be more likely to get gout in the upper extremities.9Dirken-Heukensfeldt KJ, Teunissen TA, van de Lisdonk H, Lagro-Janssen AL. "Clinical features of women with gout arthritis." A systematic review. Clin Rheumatol. 2010;29(6):575-582. doi: 10.1007/s10067-009-1362-1
While women are less likely to get gout, they are more likely to have multiple joints affected by gout.13Roddy E. Revisiting the pathogenesis of podagra: why does gout target the foot?. J Foot Ankle Res. 2011;4(1):13. Published 2011 May 13. doi: 10.1186/1757-1146-4-13
How a Gout Flare-Up Develops
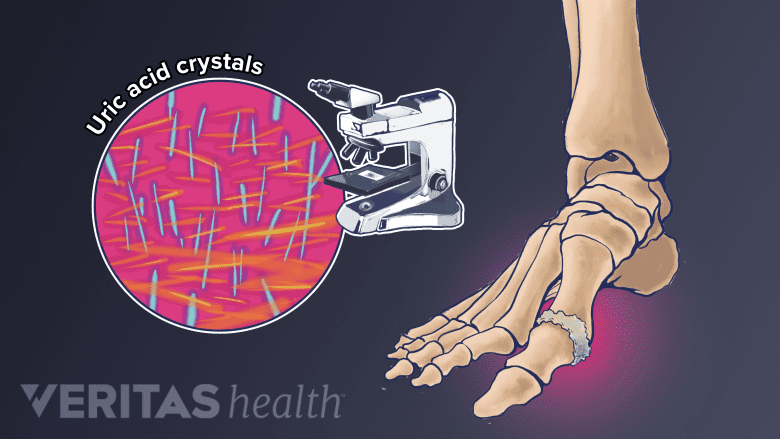
Gout occurs when excessive uric acid crystalizes in the joint and causes inflammation.
Gout results from a build-up of uric acid crystals (monosodium urate crystals) in a joint. These needle-like, microscopic crystals collect in the soft tissue of a joint, causing pain that can be excruciating, as well as swelling, redness, and warmth.
How uric acid crystals form
The build-up of uric acid crystals begins with purines, a chemical compound found in many foods.
- When the body metabolizes purines, it produces a substance called uric acid.
- The uric acid enters the bloodstream.
- The kidneys filter the blood and normally filter out excess uric acid. This uric acid is then excreted via urine (70%) or stool (30%).10Scott JT, Pollard AC. Uric acid excretion in the relatives of patients with gout. Ann Rheum Dis. 1970 Jul;29(4):397-400. Review. PubMed PMID: 4916770; PubMed Central PMCID: PMC1031324. DOI: 10.1136/ard.29.4.397
- If the kidneys cannot adequately filter out excess uric acid, or if the body produces too much uric acid, there will be too much uric acid in the bloodstream.
- Too much uric acid in the bloodstream is called hyperuricemia.
- In some people, hyperuricemia leads to the formation of uric acid crystals that collect in joint tissue, leading to painful symptoms.
An inability to adequately process and excrete uric acid accounts for an estimated 90% of gout cases.9Dirken-Heukensfeldt KJ, Teunissen TA, van de Lisdonk H, Lagro-Janssen AL. "Clinical features of women with gout arthritis." A systematic review. Clin Rheumatol. 2010;29(6):575-582. doi: 10.1007/s10067-009-1362-1 Other cases occur because a body produces too much uric acid.
Read more about Hyperuricemia - High Uric Acid Levels and Gout
Why Flare-Ups Happen at Night
It is not uncommon for gout to flare-up in the middle of the night, waking a person from a sound sleep. One research study of more than 700 gout patients found that flare-ups were 2.4 times more likely between midnight and 8 am than between 8 am and 4 pm.11Choi HK, Niu J, Neogi T, et al. Nocturnal risk of gout attacks. Arthritis Rheumatol. 2015;67(2):555-562. doi: 10.1002/art.38917
Researchers theorize gout attacks often occur at night because:
- Uric acid is more likely to form crystals at lower temperatures. The body’s temperature drops slightly during sleep, encouraging the formation of crystals.12Neogi T, Chen C, Niu J, et al. Relation of temperature and humidity to the risk of recurrent gout attacks. Am J Epidemiol. 2014;180(4):372-377. DOI: 10.1093/aje/kwu147,13Roddy E. Revisiting the pathogenesis of podagra: why does gout target the foot?. J Foot Ankle Res. 2011;4(1):13. Published 2011 May 13. doi: 10.1186/1757-1146-4-13
- Breathing rates slow down during sleep, and the lungs expel less carbon dioxide. Excess carbon dioxide can cause the blood to become slightly more acidic. This condition, called respiratory acidosis, may encourage the formation of uric acid crystals.14Martillo MA, Nazzal L, Crittenden DB. The crystallization of monosodium urate. Curr Rheumatol Rep. 2014;16(2):400. DOI: 10.1007/s11926-013-0400-9
- People with sleep apnea take in less oxygen, which can lead to an increase in the body’s production of purines and cause hyperuricemia.15Zhang Y, Peloquin CE, Dubreuil M, et al. Sleep Apnea and the Risk of Incident Gout: A Population-Based, Body Mass Index-Matched Cohort Study. Arthritis Rheumatol. 2015;67(12):3298-3302. doi: 10.1002/art.39330,17Gout. Medline Plus. US National Library of Medicine. Last Reviewed April 8, 2019. Accessed July 16, 2020. https://medlineplus.gov/ency/article/000422.htm#:~:text=It%20occurs%20when%20uric%20acid,one%20joint%20may%20be%20affected.
- The body’s cortisone levels tend to dip while sleeping. Cortisone suppresses inflammation, and a dip in cortisone may contribute to gouty inflammation.16Abhishek A, Valdes AM, Jenkins W, Zhang W, Doherty M. Triggers of acute attacks of gout, does age of gout onset matter? A primary care based cross-sectional study. PLoS One. 2017;12(10):e0186096. Published 2017 Oct 12. doi: 10.1371/journal.pone.0186096,17Gout. Medline Plus. US National Library of Medicine. Last Reviewed April 8, 2019. Accessed July 16, 2020. https://medlineplus.gov/ency/article/000422.htm#:~:text=It%20occurs%20when%20uric%20acid,one%20joint%20may%20be%20affected.
- Overnight dehydration may facilitate hyperuricemia and/or increase the concentration of crystals in the joint fluid.16Abhishek A, Valdes AM, Jenkins W, Zhang W, Doherty M. Triggers of acute attacks of gout, does age of gout onset matter? A primary care based cross-sectional study. PLoS One. 2017;12(10):e0186096. Published 2017 Oct 12. doi: 10.1371/journal.pone.0186096,17Gout. Medline Plus. US National Library of Medicine. Last Reviewed April 8, 2019. Accessed July 16, 2020. https://medlineplus.gov/ency/article/000422.htm#:~:text=It%20occurs%20when%20uric%20acid,one%20joint%20may%20be%20affected.
More research is needed in this area.
Gout Attack vs. Chronic Gout
It is possible to have a gout flare-up and never experience another. Repeated instances of acute gout are called chronic gout17Gout. Medline Plus. US National Library of Medicine. Last Reviewed April 8, 2019. Accessed July 16, 2020. https://medlineplus.gov/ency/article/000422.htm#:~:text=It%20occurs%20when%20uric%20acid,one%20joint%20may%20be%20affected..
The treatment goals for a gout attack are different than those for chronic gout. When treating a gout attack, the goal is to relieve pain and inflammation. When treating chronic gout, the goal is to prevent future gout attacks and long-term joint damage.
While some people with chronic gout may get frequent gout attacks, others may have years in between attacks. If chronic gout is not treated, attacks may become more frequent and/or last longer.
Left untreated, a gout attack will usually resolve itself within a few days or weeks. Chronic gout can permanently damage a joint’s tissues and decrease its range of motion. For this reason, it is important to recognize symptoms, understand risk factors, get an accurate diagnosis, and treat and prevent gout.
- 1 Zhu Y, Pandya BJ, Choi HK. Prevalence of gout and hyperuricemia in the US general population: the National Health and Nutrition Examination Survey 2007-2008. Arthritis Rheum 2011;63(10):3136–41. As cited in Sidari A, Hill E. Diagnosis and Treatment of Gout and Pseudogout for Everyday Practice. Prim Care. 2018;45(2):213-236. doi:10.1016/j.pop.2018.02.004
- 2 Sidari A, Hill E. Diagnosis and Treatment of Gout and Pseudogout for Everyday Practice. Prim Care. 2018;45(2):213-236. doi:10.1016/j.pop.2018.02.004
- 3 Riddell CM, Elliott M, Cairns, AP. An Unusual "Gouty" Case of Back Pain and Fever. J Rheumatol October 2008 35(10):2076-2077 PMID: 18843766
- 4 Bang SY, Jeong JH, Joo KB, Jun JB, Sung YK. A Case of the Lumbar Spine Involvement and Sacroiliitis in a Patient with Gout. J Korean Rheum Assoc. 2009 Dec;16(4):318-322. https://doi.org/10.4078/jkra.2009.16.4.318
- 5 Mantle B, Gross P, Lopez-Ben R, Alarcón GS. Hip pain as the presenting manifestation of acute gouty sacroiliitis. J Clin Rheumatol. 2001 Apr;7(2):112-4. PubMed PMID: 17039107.
- 6 Konatalapalli RM, Demarco PJ, Jelinek JS, Murphey M, Gibson M, Jennings B, Weinstein A. Gout in the axial skeleton. J Rheumatol. 2009 Mar;36(3):609-13. doi: 10.3899/jrheum.080374. Epub 2009 Feb 4. PubMed PMID: 19208604.
- 7 Klauser AS, Halpern EJ, Strobl S, et al. Gout of hand and wrist: the value of US as compared with DECT. Eur Radiol. 2018;28(10):4174-4181. DOI: 10.1007/s00330-018-5363-9
- 8 Slobodonick A, Toprover M, Pillinger M. Crystal Arthritis. In: Efthimiou P, ed. Absolute Rheumatology Review. Springer Nature Switzerland AG; 2020; chap 15. Accessed September 15, 2020. https://doi.org/10.1007/978-3-030-23022-7_15
- 10 Scott JT, Pollard AC. Uric acid excretion in the relatives of patients with gout. Ann Rheum Dis. 1970 Jul;29(4):397-400. Review. PubMed PMID: 4916770; PubMed Central PMCID: PMC1031324. DOI: 10.1136/ard.29.4.397
- 9 Dirken-Heukensfeldt KJ, Teunissen TA, van de Lisdonk H, Lagro-Janssen AL. "Clinical features of women with gout arthritis." A systematic review. Clin Rheumatol. 2010;29(6):575-582. doi: 10.1007/s10067-009-1362-1
- 13 Roddy E. Revisiting the pathogenesis of podagra: why does gout target the foot?. J Foot Ankle Res. 2011;4(1):13. Published 2011 May 13. doi: 10.1186/1757-1146-4-13
- 11 Choi HK, Niu J, Neogi T, et al. Nocturnal risk of gout attacks. Arthritis Rheumatol. 2015;67(2):555-562. doi: 10.1002/art.38917
- 12 Neogi T, Chen C, Niu J, et al. Relation of temperature and humidity to the risk of recurrent gout attacks. Am J Epidemiol. 2014;180(4):372-377. DOI: 10.1093/aje/kwu147
- 14 Martillo MA, Nazzal L, Crittenden DB. The crystallization of monosodium urate. Curr Rheumatol Rep. 2014;16(2):400. DOI: 10.1007/s11926-013-0400-9
- 15 Zhang Y, Peloquin CE, Dubreuil M, et al. Sleep Apnea and the Risk of Incident Gout: A Population-Based, Body Mass Index-Matched Cohort Study. Arthritis Rheumatol. 2015;67(12):3298-3302. doi: 10.1002/art.39330
- 17 Gout. Medline Plus. US National Library of Medicine. Last Reviewed April 8, 2019. Accessed July 16, 2020. https://medlineplus.gov/ency/article/000422.htm#:~:text=It%20occurs%20when%20uric%20acid,one%20joint%20may%20be%20affected.
- 16 Abhishek A, Valdes AM, Jenkins W, Zhang W, Doherty M. Triggers of acute attacks of gout, does age of gout onset matter? A primary care based cross-sectional study. PLoS One. 2017;12(10):e0186096. Published 2017 Oct 12. doi: 10.1371/journal.pone.0186096

