Research suggests that arthritis inflammation and pain are connected to problems in the gut microbiome. People can cultivate healthier gut microbiomes through their diets by:
- Eating a healthy, whole foods diet. A healthy gut depends on eating whole foods, including lots of vegetables—especially leafy greens—as well as fruits and whole grains. Healthy whole foods help beneficial bacteria thrive and starve out “bad” bacteria. Probiotics and prebiotics may help, too, especially when antibiotics are taken.1Issa I, Moucari R. Probiotics for antibiotic-associated diarrhea: do we have a verdict?. World J Gastroenterol. 2014;20(47):17788-95.,2Johnson LP, Walton GE, Psichas A, Frost GS, Gibson GR, Barraclough TG. Prebiotics Modulate the Effects of Antibiotics on Gut Microbial Diversity and Functioning in Vitro. Nutrients. 2015;7(6):4480-97.
- Avoiding foods that trigger inflammation. Foods typical of the Western diet, such as processed or sugary foods, trigger inflammation. Even seemingly healthy foods, such as eggs and milk, can trigger inflammation in some people.
Each person with arthritis has his or her own set of trigger foods. Because every person is different, individuals are advised to do an elimination diet and keep a food diary.
In This Article:
- Improving the Gut Microbiome and Arthritis Symptoms with Diet
- The Science Behind Leaky Gut, the Gut Microbiome, and Arthritis
- Foods for a Healthier Gut and Less Arthritis Pain
An Elimination Diet Can Identify Triggers of Arthritis Pain
The best way to identify foods that trigger inflammation is to do an elimination diet. An elimination diet begins by eating only foods that rarely cause inflammation in anyone, such as leafy greens, quinoa, sweet potatoes, and chicken. These foods are called baseline foods.
After a few weeks of eating only baseline foods, other foods are added back into the diet one by one. For example, a person might add eggs back into his or her diet, eating them two times a day for 3 or 4 days. The patient monitors his or her symptoms during these days. If there is no reaction, eggs can continue to be eaten.
This methodical way of adding new foods back in makes it easy to identify what foods cause inflammation and arthritis pain.
Foods to Eliminate
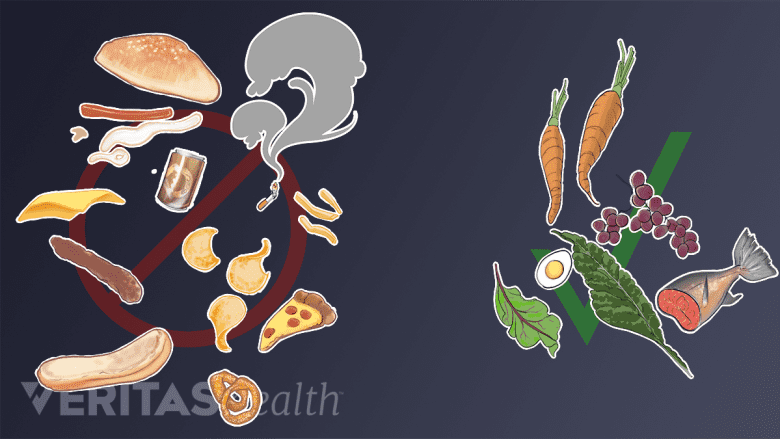
Some foods are best avoided to help reduce inflammation, while others may be helpful.
The foods listed below are believed most likely to trigger arthritis inflammation and should be avoided during the first three weeks of an elimination diet.
- Gluten, including all wheat products, such as breads and pastas
- Dairy products, such as milk, yogurt, cheese, and sour cream
- Soy, including edamame, tofu, tempeh, miso, tamari, and many meat substitute products
- Corn, including corn chips, tortillas, grits, and corn derivatives, such as corn syrups and starches
- Eggs, including dishes that contain eggs, such as baked goods, breaded and fried foods, creams, and puddings
- Nightshade vegetables, including tomatoes, potatoes, eggplant and peppers
- Processed foods, especially processed baked goods, such as cookies, cakes, and bagels
- Sugars, including any products that contain traditional sugar, brown sugar, corn syrup, sucrose or other added sweeteners (a little bit of honey or molasses may be okay)
- Alcohol, including beer, wine, hard liquors and spirits
- Certain meats, including red meat, smoked meats, deli meats and pork. Turkey, chicken and fish are allowed.
An Anti-Inflammatory Diet for Arthritis
People on this elimination diet are advised to wait 3 to 4 days before reintroducing each group.
Keep in mind this is just one example of an elimination diet for people with arthritis and autoimmune issues. Other diets provide different guidelines. For example, certain other elimination diets recommend avoiding all meats and oils and do not require eliminating nightshade vegetables. (The Arthritis Foundation does not support the position that nightshade plants cause arthritis inflammation but acknowledges that some people are sensitive to certain vegetables.)
Foods to Eat
Evidence suggests that the best diet to reduce arthritis pain is:
Low glycemic. Foods that do not cause a rapid elevation in blood sugar are considered low-glycemic foods. These foods contain lots of fiber and break down slowly. Examples include potatoes, oatmeal, vegetables, and most fruits are considered low-glycemic foods. (Fruit juices typically do not have a lot of fiber and can be high-glycemic.)
High in fiber. Fiber is a prebiotic—meaning it helps beneficial microbes thrive in the gut. People who eat foods high in fiber produce lots of short chain fatty acids, which can help treat gut dysbiosis. Moreover, recent research suggests that people who eat high-fiber diets have less osteoarthritis pain.3Dai Z, Niu J, Zhang Y, Jacques P, Felson DT. Dietary intake of fibre and risk of knee osteoarthritis in two US prospective cohorts. Ann Rheum Dis. 2017;76(8):1411-1419.,4Dai Z, Lu N, Niu J, Felson DT, Zhang Y. Dietary Fiber Intake in Relation to Knee Pain Trajectory. Arthritis Care Res (Hoboken). 2017;69(9):1331-1339.
High in polyphenols. Polyphenols are naturally occurring chemicals in plant-based foods. These chemicals counteract free radicals, which can cause damage to the body’s tissues. Polyphenols are found in a wide variety of foods, including vegetables, fruits, spices (particularly clove5Pérez-jiménez J, Neveu V, Vos F, Scalbert A. Identification of the 100 richest dietary sources of polyphenols: an application of the Phenol-Explorer database. Eur J Clin Nutr. 2010;64 Suppl 3:S112-20.), and even teas and coffee.
High in healthy fats. Avocadoes, nuts, seeds, and olives are all plant-based whole foods high in healthy fats. Fish, such as salmon, and some oils, such as olive oil, are also considered to be sources of health fats by most experts.
Low in sugar. A whole foods, plant-based diet will be naturally low in sugars, such corn syrup, which is known to cause inflammation.
What Are Anti-Inflammatory Foods?
Unprocessed. Unprocessed foods are direct products of nature—fruits, vegetables, and whole grains. Processed foods, such as packaged cereals and cookies, tend to be low in fiber and high in sugar. Processed foods also typically contain additives, such as polysorbate 80, that enhance taste, texture, and shelf life. These additives can lead inflammation in the gut.6Chassaing B, Van de wiele T, De bodt J, Marzorati M, Gewirtz AT. Dietary emulsifiers directly alter human microbiota composition and gene expression ex vivo potentiating intestinal inflammation. Gut. 2017;66(8):1414-1427.,7Cani PD, Everard A. Keeping gut lining at bay: impact of emulsifiers. Trends Endocrinol Metab. 2015;26(6):273-4.
Low in or free of dairy. Dairy products are a great source of calcium and other nutrients, but they also happen to cause inflammation in many people. People who have conducted an elimination diet and found that dairy products do not affect their symptoms may choose to eat a limited amount of dairy foods.
Low in or free of red meat. Eating turkey, chicken and fish is okay, but people are advised to avoid processed deli meats and red meats. During digestion, certain bacteria in the gut feed on red meat, leading to the production of a chemical called trimethylamine-N-oxide (TMAO).8Koeth RA, Wang Z, Levison BS, et al. Intestinal microbiota metabolism of L-carnitine, a nutrient in red meat, promotes atherosclerosis. Nat Med. 2013;19(5):576-85. TMAO is associated with vascular inflammation and heart disease.9Seldin MM, Meng Y, Qi H, et al. Trimethylamine N-Oxide Promotes Vascular Inflammation Through Signaling of Mitogen-Activated Protein Kinase and Nuclear Factor-κB. J Am Heart Assoc. 2016;5(2)
High in Omega 3 fatty acids. Several studies have associated omega 3 intake with arthritis symptom relief.10Akbar U, Yang M, Kurian D, Mohan C. Omega-3 Fatty Acids in Rheumatic Diseases: A Critical Review. J Clin Rheumatol. 2017;23(6):330-339. Omega 3s are found naturally in many foods, including but not limited to flax seed, chia seed, seaweed,11Van ginneken VJ, Helsper JP, De visser W, Van keulen H, Brandenburg WA. Polyunsaturated fatty acids in various macroalgal species from North Atlantic and tropical seas. Lipids Health Dis. 2011;10:104. walnuts, Atlantic salmon, and certain other types of fish.
Omega 3 can also be taken as a supplement, typically a fish oil product. However, people who take omega 3 supplements should not expect noticeable results without also eating a healthy diet. Why? Omega 3 absorption can be blocked by omega 6 fatty acids. Omega 6’s are found naturally in some foods, but are especially high in potato chips, pizza, processed meats, and other typical Western diet foods.
Dietary Supplements for Treating Arthritis
Again, these guidelines are based on current research and clinical experience. Different experts recommend different anti-inflammatory diets, and some may put emphasis on other dietary categories. The important point is that most of these diets share the same underlying goal of healing the gut.
Integrative Arthritis Therapies and Nutrition
It may be that be one particular diet program works best. Or, it may be that one program works for best for certain people while other programs work better for others. More research is needed in this area.
The Ins and Outs of an Anti-Inflammatory Diet
Stay committed
Until more is known, patients are advised to find a program and stick to it for a few months before deciding whether or not it works. Progress may occur suddenly or gradually; any progress is a positive indication that symptoms can be managed through diet.
Keep stress low and exercise regularly
In addition to diet, the gut microbiome is influenced by other factors, including heredity, stress, and environment. For this reason, people who are rehabilitating their guts with diet are advised to also exercise regularly, meditate, and reduce their exposure to toxins.
- 1 Issa I, Moucari R. Probiotics for antibiotic-associated diarrhea: do we have a verdict?. World J Gastroenterol. 2014;20(47):17788-95.
- 2 Johnson LP, Walton GE, Psichas A, Frost GS, Gibson GR, Barraclough TG. Prebiotics Modulate the Effects of Antibiotics on Gut Microbial Diversity and Functioning in Vitro. Nutrients. 2015;7(6):4480-97.
- 3 Dai Z, Niu J, Zhang Y, Jacques P, Felson DT. Dietary intake of fibre and risk of knee osteoarthritis in two US prospective cohorts. Ann Rheum Dis. 2017;76(8):1411-1419.
- 4 Dai Z, Lu N, Niu J, Felson DT, Zhang Y. Dietary Fiber Intake in Relation to Knee Pain Trajectory. Arthritis Care Res (Hoboken). 2017;69(9):1331-1339.
- 5 Pérez-jiménez J, Neveu V, Vos F, Scalbert A. Identification of the 100 richest dietary sources of polyphenols: an application of the Phenol-Explorer database. Eur J Clin Nutr. 2010;64 Suppl 3:S112-20.
- 6 Chassaing B, Van de wiele T, De bodt J, Marzorati M, Gewirtz AT. Dietary emulsifiers directly alter human microbiota composition and gene expression ex vivo potentiating intestinal inflammation. Gut. 2017;66(8):1414-1427.
- 7 Cani PD, Everard A. Keeping gut lining at bay: impact of emulsifiers. Trends Endocrinol Metab. 2015;26(6):273-4.
- 8 Koeth RA, Wang Z, Levison BS, et al. Intestinal microbiota metabolism of L-carnitine, a nutrient in red meat, promotes atherosclerosis. Nat Med. 2013;19(5):576-85.
- 9 Seldin MM, Meng Y, Qi H, et al. Trimethylamine N-Oxide Promotes Vascular Inflammation Through Signaling of Mitogen-Activated Protein Kinase and Nuclear Factor-κB. J Am Heart Assoc. 2016;5(2)
- 10 Akbar U, Yang M, Kurian D, Mohan C. Omega-3 Fatty Acids in Rheumatic Diseases: A Critical Review. J Clin Rheumatol. 2017;23(6):330-339.
- 11 Van ginneken VJ, Helsper JP, De visser W, Van keulen H, Brandenburg WA. Polyunsaturated fatty acids in various macroalgal species from North Atlantic and tropical seas. Lipids Health Dis. 2011;10:104.
Editor’s Top Picks
- Connections Between the Gut Microbiome and Arthritis
- Gut Microbiome Health and Diversity
- Reduce the Risk of Arthritis by Improving the Microbiome
- Video: The Best-Tasting Anti-Inflammatory Cocktail You've Never Tried
- In the Kitchen with Arthritis: Foods to Avoid
- Video: A Hearty Meal to Reduce Arthritis Inflammation

