A person who has an inflammatory arthritis, particularly a spondyloarthritis such as ankylosing spondylitis or psoriatic arthritis, may experience pain caused by changes to an enthesis (en-THEE-sis). An enthesis is the point where a ligament or tendon attaches to bone. (The plural form is entheses.)
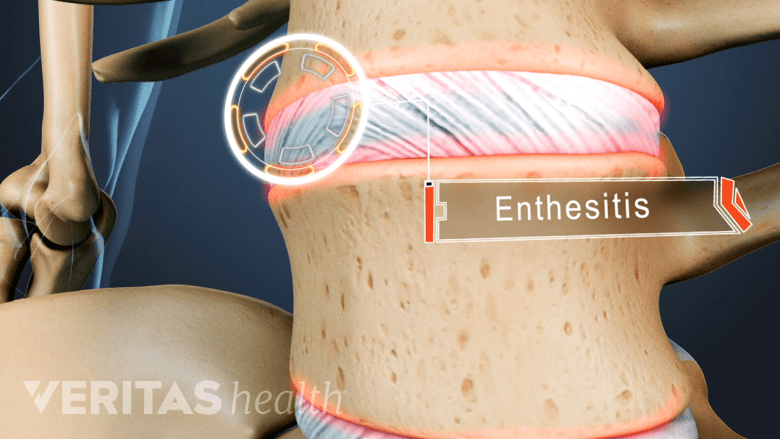
Enthesitis is the first stage in the development of ankylosing spondylitis.
Enthesopathy (en-THEE-sawp-a-thee) is the medical name for any disease or disorder affecting an enthesis. Doctors may use the terms enthesopathy and enthesitis interchangeably—“itis” implies inflammation of the enthesis.
Joints Affected by Enthesopathy
Enthesopathy most commonly affects:
- Feet/heels, especially involving the Achilles tendon (very common) and plantar fascia
- Elbows
- Shoulders
- Hips
- The facet joints that connect the spine’s vertebrae
- The sacroiliac joint between the base of the spine and the pelvis (most common in ankylosing spondylitis)
See Sacroiliac Joint Pain and Inflammation
Enthesopathy can also affect fixed joints. Fixed joints are places where two bones meet but there is little movement. For example, the joints between the breastbone and ribs are fixed joints.
See How Arthritis Causes Joint Pain
How Arthritis Is Related to Enthesopathy
A doctor who diagnoses a patient with enthesopathy will want to identify and treat the underlying cause. In many cases, the underlying cause is systemic (body-wide) inflammation related to arthritis. As inflammation takes place, one or more entheses may become irritated and cause pain.
Arthritic conditions associated with enthesopathy include but are not limited to:
- Ankylosing spondylitis
- Inflammatory Arthritis
- Psoriatic arthritis
- Septic arthritis
Trauma and enthesopathy
It is possible for enthesopathy to result from a torn tendon or an avulsion fracture (in which a ligament’s or tendon’s enthesis breaks off with a bit of surrounding bone). But in most cases, enthesopathy usually does not result from traumatic injuries.
Treatment for Enthesopathy
There is no specific treatment for enthesopathy, but there are treatments for the underlying diseases that lead to it. These treatments may involve a combination of exercise, activity modification, and medication. Medications can be discussed as a treatment option with your rheumatologist.

