It is common for rheumatoid arthritis and low back pain to occur together.1Kawaguchi Y, Matsuno H, Kanamori M, Ishihara H, Ohmori K, Kimura T. Radiologic findings of the lumbar spine in patients with rheumatoid arthritis, and a review of pathologic mechanisms. J Spinal Disord Tech. 2003 Feb;16(1):38-43. doi: 10.1097/00024720-200302000-00007. PMID: 12571483.,2Baykara RA, Bozgeyik Z, Akgul O, Ozgocmen S. Low back pain in patients with rheumatoid arthritis: clinical characteristics and impact of low back pain on functional ability and health related quality of life. J Back Musculoskelet Rehabil. 2013;26(4):367-74. doi: 10.3233/BMR-130393. PMID: 23948822.,3Munakomi S, Foris LA, Varacallo M. Spinal Stenosis And Neurogenic Claudication. [Updated 2021 Feb 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430872/ While low back pain is rarely a direct symptom of RA, the two conditions may be linked.
This article describes the connection between rheumatoid arthritis and low back pain, including sciatica. Also discussed are ways to safely relieve low back pain at home when RA is present.
In This Article:
- Rheumatoid Arthritis and Low Back Pain
- Relief for Low Back Pain with Rheumatoid Arthritis
RA Rarely Attacks the Joints of the Lower Spine
Rheumatoid arthritis causes the body’s immune system to attack the lining of synovial joints. However, it is rare for RA to attack the synovial joints of the lower spine,4Riaz S, Kontzias A. Rheumatoid Arthritis In: Efthimiou P, ed. Absolute Rheumatology Review. Electronic book. Springer; 2020: 125-149. Accessed May 12, 2021. https://doi.org/10.1007/978-3-030-23022-7 which connect vertebrae to each other (facet joints) and to the pelvis (sacroiliac joints).
Rheumatoid arthritis is more likely to affect the lower spine in other ways.
RA May Contribute to Low Back Pain and Sciatica
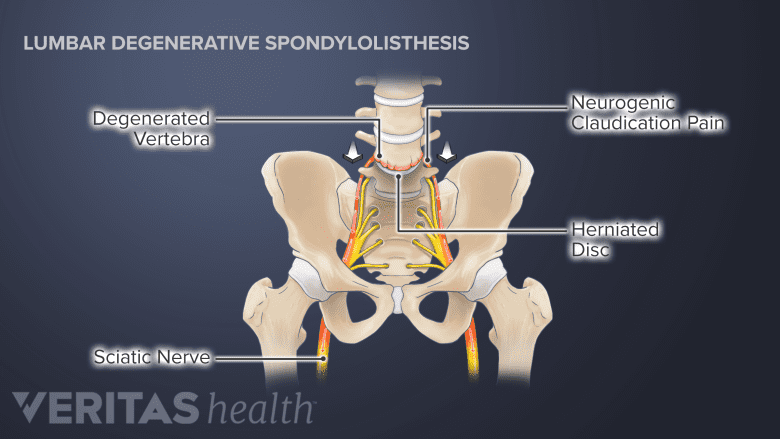
Spinal degeneration may result in instability and the forward slippage of the vertebra, causing neurogenic claudication pain.
While rheumatoid arthritis rarely attacks the joints of the lower spine, it may cause degenerative changes that trigger or worsen low back pain. These changes include the weakening or loss of bone and other tissues. In particular:
- RA inflammation may play a role in deteriorating bone and soft tissue where vertebrae meet intervertebral discs (endplates)
- RA raises the risk for osteoporosis and low bone mineral density, which increases the chances for bone erosion and vertebral fractures
One or both of these changes may lead to inflammation and muscle strain that cause low back pain. The changes may also lead to a loss of space between vertebrae that, left untreated, cause problems such as scoliosis, spondylolisthesis, neurogenic claudication, radiculopathy, or increased instability in the spine.5Joo P, Ge L, Mesfin A. Surgical Management of the Lumbar Spine in Rheumatoid Arthritis. Global Spine J. 2020;10(6):767-774. doi:10.1177/2192568219886267
Rheumatoid arthritis and sciatica
The term sciatica describes the symptoms that occur when the sciatic nerve is pinched or irritated (it is a type of radiculopathy). These symptoms may include pain, tingling, numbness, and weakness that radiate along the sciatic nerve, affecting the buttocks, the back of the leg, and the foot.
Sciatica is not a medical diagnosis. It can be caused by a variety of conditions, including those associated with RA, such as spondylolisthesis.
To relieve sciatica, the underlying cause(s) must be treated.
Low Back Pain Is Less Severe with RA
Interestingly, low back pain may be less severe for people with RA.2Baykara RA, Bozgeyik Z, Akgul O, Ozgocmen S. Low back pain in patients with rheumatoid arthritis: clinical characteristics and impact of low back pain on functional ability and health related quality of life. J Back Musculoskelet Rehabil. 2013;26(4):367-74. doi: 10.3233/BMR-130393. PMID: 23948822. Experts hypothesize that:
- Anti-inflammatory drugs taken to treat RA may also reduce low back pain
- RA causes physical changes in the spine that suppress the growth of bone spurs, thereby reducing the risk of pinched nerves.
More research is needed on this topic.
Increased risk for disability, poor quality of life, and depression
While low back pain may not be severe, its effects can be significant. People who are diagnosed with both RA and low back pain tend to report higher rates of disability, lower quality of life, and more symptoms of depression.2Baykara RA, Bozgeyik Z, Akgul O, Ozgocmen S. Low back pain in patients with rheumatoid arthritis: clinical characteristics and impact of low back pain on functional ability and health related quality of life. J Back Musculoskelet Rehabil. 2013;26(4):367-74. doi: 10.3233/BMR-130393. PMID: 23948822.,6Kothe R. Rückenschmerz bei rheumatoider Arthritis [Low back pain in rheumatoid arthritis], abstract only. Z Rheumatol. 2017 Dec;76(10):869-875. German. doi: 10.1007/s00393-017-0363-8. PMID: 28875320.
Treatment to alleviate chronic pain and improve everyday function may increase quality of life and reduce symptoms of depression.
Rheumatoid Arthritis May Cause Neck Pain
In contrast to the joints in the low spine, the joints in the neck are particularly susceptible to rheumatoid arthritis. About half the people with RA experience inflammation in the neck’s cervical facet joints.4Riaz S, Kontzias A. Rheumatoid Arthritis In: Efthimiou P, ed. Absolute Rheumatology Review. Electronic book. Springer; 2020: 125-149. Accessed May 12, 2021. https://doi.org/10.1007/978-3-030-23022-7
Symptoms of RA in the neck
When the cervical facet joints are inflamed, they may cause pain, tenderness, stiffness, and swelling in the neck and base of the skull. Headaches may be common. If the joint deterioration becomes severe it can affect nerve roots and cause pain to radiate down one or both arms.
Certain Factors Increase the Risk of Low Back Pain
Experts estimate that rheumatoid arthritis doubles the risk of developing low back pain.2Baykara RA, Bozgeyik Z, Akgul O, Ozgocmen S. Low back pain in patients with rheumatoid arthritis: clinical characteristics and impact of low back pain on functional ability and health related quality of life. J Back Musculoskelet Rehabil. 2013;26(4):367-74. doi: 10.3233/BMR-130393. PMID: 23948822.,7Miura K, Morita O, Hirano T, Watanabe K, Fujisawa J, Kondo N, Netsu T, Hanyu T, Shobugawa Y, Endo N. Prevalence of and factors associated with dysfunctional low back pain in patients with rheumatoid arthritis. Eur Spine J. 2019 May;28(5):976-982. doi: 10.1007/s00586-019-05938-x. Epub 2019 Mar 8. PMID: 30850879. Specific factors that raise the risk of developing low back pain that affects day-to-day living include:
Greater disease activity
The more active RA is in the body (as measured by Disease Activity Scores) the more likely back pain may be a problem.7Miura K, Morita O, Hirano T, Watanabe K, Fujisawa J, Kondo N, Netsu T, Hanyu T, Shobugawa Y, Endo N. Prevalence of and factors associated with dysfunctional low back pain in patients with rheumatoid arthritis. Eur Spine J. 2019 May;28(5):976-982. doi: 10.1007/s00586-019-05938-x. Epub 2019 Mar 8. PMID: 30850879.,8Masamoto K, Otsuki B, Fujibayashi S, Shima K, Ito H, Furu M, Hashimoto M, Tanaka M, Lyman S, Yoshitomi H, Tanida S, Mimori T, Matsuda S. Factors influencing spinal sagittal balance, bone mineral density, and Oswestry Disability Index outcome measures in patients with rheumatoid arthritis. Eur Spine J. 2018 Feb;27(2):406-415. doi: 10.1007/s00586-017-5401-3. Epub 2017 Nov 28. PMID: 29185111.,9Yamada K, Suzuki A, Takahashi S et al (2015) Severe low back pain in patients with rheumatoid arthritis is associated with Dis- ease Activity Score but not with radiological findings on plain X-rays. Mod Rheumatol 25:56–61. https://doi.org/10.3109/1439 7595.2014.924187 Using the treat-to-target strategy or other approaches to keep RA under control is encouraged.
Less methotrexate use
Taking methotrexate, a disease-modifying anti-rheumatic drug (DMARD) often prescribed to treat RA, may be associated with less low back pain.7Miura K, Morita O, Hirano T, Watanabe K, Fujisawa J, Kondo N, Netsu T, Hanyu T, Shobugawa Y, Endo N. Prevalence of and factors associated with dysfunctional low back pain in patients with rheumatoid arthritis. Eur Spine J. 2019 May;28(5):976-982. doi: 10.1007/s00586-019-05938-x. Epub 2019 Mar 8. PMID: 30850879.
Corticosteroid use
Prednisone and other corticosteroids used to control RA flares have been linked to a greater risk for low back pain.7Miura K, Morita O, Hirano T, Watanabe K, Fujisawa J, Kondo N, Netsu T, Hanyu T, Shobugawa Y, Endo N. Prevalence of and factors associated with dysfunctional low back pain in patients with rheumatoid arthritis. Eur Spine J. 2019 May;28(5):976-982. doi: 10.1007/s00586-019-05938-x. Epub 2019 Mar 8. PMID: 30850879.,8Masamoto K, Otsuki B, Fujibayashi S, Shima K, Ito H, Furu M, Hashimoto M, Tanaka M, Lyman S, Yoshitomi H, Tanida S, Mimori T, Matsuda S. Factors influencing spinal sagittal balance, bone mineral density, and Oswestry Disability Index outcome measures in patients with rheumatoid arthritis. Eur Spine J. 2018 Feb;27(2):406-415. doi: 10.1007/s00586-017-5401-3. Epub 2017 Nov 28. PMID: 29185111. Not all research supports this connection, and the topic is considered controversial.
A history of vertebral fracture(s)7Miura K, Morita O, Hirano T, Watanabe K, Fujisawa J, Kondo N, Netsu T, Hanyu T, Shobugawa Y, Endo N. Prevalence of and factors associated with dysfunctional low back pain in patients with rheumatoid arthritis. Eur Spine J. 2019 May;28(5):976-982. doi: 10.1007/s00586-019-05938-x. Epub 2019 Mar 8. PMID: 30850879.
Vertebrae may be weakened due to RA and possible corticosteroid use, making them more susceptible to fractures. A fractured vertebra may result in changes that cause low back pain, even after the bone has healed.
Higher body mass index (BMI)7Miura K, Morita O, Hirano T, Watanabe K, Fujisawa J, Kondo N, Netsu T, Hanyu T, Shobugawa Y, Endo N. Prevalence of and factors associated with dysfunctional low back pain in patients with rheumatoid arthritis. Eur Spine J. 2019 May;28(5):976-982. doi: 10.1007/s00586-019-05938-x. Epub 2019 Mar 8. PMID: 30850879.
Excess weight puts strain on the spine and increases the likelihood of developing low back pain. Excess weight is also associated with increased body-wide inflammation, which may exacerbate RA pain and low back symptoms.
Differences in skeletal alignment and posture
RA with low back pain is associated with poor skeletal alignment.7Miura K, Morita O, Hirano T, Watanabe K, Fujisawa J, Kondo N, Netsu T, Hanyu T, Shobugawa Y, Endo N. Prevalence of and factors associated with dysfunctional low back pain in patients with rheumatoid arthritis. Eur Spine J. 2019 May;28(5):976-982. doi: 10.1007/s00586-019-05938-x. Epub 2019 Mar 8. PMID: 30850879. For example, a hunched back or a loss of the normal curve in the lower spine is linked to low back pain.
Poor pelvic alignment—the angle at which the pelvic bone is positioned during standing and sitting—can also cause low back pain or make existing pain worse.
Some of the factors listed above can be modified. Taking steps to change them may be part of a treatment plan.
- 1 Kawaguchi Y, Matsuno H, Kanamori M, Ishihara H, Ohmori K, Kimura T. Radiologic findings of the lumbar spine in patients with rheumatoid arthritis, and a review of pathologic mechanisms. J Spinal Disord Tech. 2003 Feb;16(1):38-43. doi: 10.1097/00024720-200302000-00007. PMID: 12571483.
- 2 Baykara RA, Bozgeyik Z, Akgul O, Ozgocmen S. Low back pain in patients with rheumatoid arthritis: clinical characteristics and impact of low back pain on functional ability and health related quality of life. J Back Musculoskelet Rehabil. 2013;26(4):367-74. doi: 10.3233/BMR-130393. PMID: 23948822.
- 3 Munakomi S, Foris LA, Varacallo M. Spinal Stenosis And Neurogenic Claudication. [Updated 2021 Feb 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430872/
- 4 Riaz S, Kontzias A. Rheumatoid Arthritis In: Efthimiou P, ed. Absolute Rheumatology Review. Electronic book. Springer; 2020: 125-149. Accessed May 12, 2021. https://doi.org/10.1007/978-3-030-23022-7
- 5 Joo P, Ge L, Mesfin A. Surgical Management of the Lumbar Spine in Rheumatoid Arthritis. Global Spine J. 2020;10(6):767-774. doi:10.1177/2192568219886267
- 6 Kothe R. Rückenschmerz bei rheumatoider Arthritis [Low back pain in rheumatoid arthritis], abstract only. Z Rheumatol. 2017 Dec;76(10):869-875. German. doi: 10.1007/s00393-017-0363-8. PMID: 28875320.
- 7 Miura K, Morita O, Hirano T, Watanabe K, Fujisawa J, Kondo N, Netsu T, Hanyu T, Shobugawa Y, Endo N. Prevalence of and factors associated with dysfunctional low back pain in patients with rheumatoid arthritis. Eur Spine J. 2019 May;28(5):976-982. doi: 10.1007/s00586-019-05938-x. Epub 2019 Mar 8. PMID: 30850879.
- 8 Masamoto K, Otsuki B, Fujibayashi S, Shima K, Ito H, Furu M, Hashimoto M, Tanaka M, Lyman S, Yoshitomi H, Tanida S, Mimori T, Matsuda S. Factors influencing spinal sagittal balance, bone mineral density, and Oswestry Disability Index outcome measures in patients with rheumatoid arthritis. Eur Spine J. 2018 Feb;27(2):406-415. doi: 10.1007/s00586-017-5401-3. Epub 2017 Nov 28. PMID: 29185111.
- 9 Yamada K, Suzuki A, Takahashi S et al (2015) Severe low back pain in patients with rheumatoid arthritis is associated with Dis- ease Activity Score but not with radiological findings on plain X-rays. Mod Rheumatol 25:56–61. https://doi.org/10.3109/1439 7595.2014.924187

