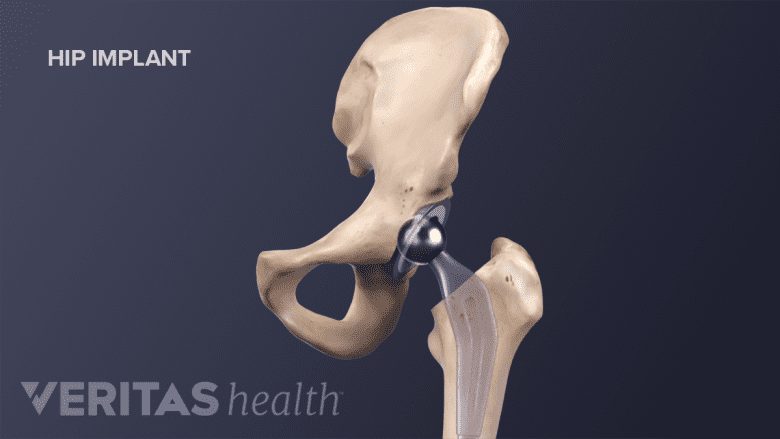
The goal of most hip replacements is to alleviate hip pain due to arthritis. During surgery, the orthopedic surgeon resurfaces the bones that form the ball-and-socket of the hip joint. When complete, the prosthetic ball fits into the prosthetic hip socket to create a new hip joint.
After recovery, people with hip replacements typically report1Carol A. Mancuso, Jennifer Jout, Eduardo A. Salvati, Thomas P. Sculco; Fulfillment of Patients' Expectations for Total Hip Arthroplasty. The Journal of Bone & Joint Surgery. 2009 Sep;91(9):2073-2078.:
- Less or no nighttime hip pain
- An elimination or reduction in pain medications
- Improved ability to walk
- Improved ability work and participate in recreational or social activities
Total hip replacement surgery is sometimes called total hip arthroplasty. More than 90% of patients who have had elective total hip replacement surgery say they would make the same choice again.1Carol A. Mancuso, Jennifer Jout, Eduardo A. Salvati, Thomas P. Sculco; Fulfillment of Patients' Expectations for Total Hip Arthroplasty. The Journal of Bone & Joint Surgery. 2009 Sep;91(9):2073-2078.
In This Article:
- Total Hip Replacement for Hip Arthritis
- Indications and Eligibility for Total Hip Replacement Surgery
- Total Hip Replacement Surgical Procedure
- Additional Facts and Considerations for Total Hip Replacement Surgery
- Total Hip Replacement Surgery Recovery
- Total Hip Replacement Surgery Risks and Complications
- Total Hip Replacement Surgery Animation
Try Nonsurgical Treatments First
While hip replacement surgery is considered one of the most reliably successful surgeries available today,2Harkess, JW and Crockarell, JR Jr. Arthroplasty of the Hip. Campbell’s Operative Orthopedics, 13th edition. Philidelphia, PA. Elsevier, 2017: 167-321. it is a major surgery. After surgery, patients often benefit from a course of physical therapy. A full recovery can take 3 to 12 months.
Nonsurgical treatments, such as medication and joint-strengthening physical therapy, are strongly recommended before considering total hip replacement surgery.
See Hip Osteoarthritis Treatment
The Lifespan of a Hip Replacement
Research suggests3Bayliss LE, Culliford D, Monk AP, et al. The effect of patient age at intervention on risk of implant revision after total replacement of the hip or knee: a population-based cohort study [published correction appears in Lancet. 2017 Apr 8;389(10077):1398]. Lancet. 2017;389(10077):1424–1430. doi:10.1016/S0140-6736(17)30059-4 95% of hip replacements last 10 years or longer and 85% last 20 years or longer. This longevity can be attributed to improvements in both surgical technique and implant design.
Patients can help extend the life of their hip replacements by sticking to their physical therapy routines and avoiding high-impact activities.
Revision Hip Replacement
If a new hip prothesis becomes loose, breaks, wears out, or repeatedly dislocates, then a second surgery called a revision total hip replacement is often recommended.
The complication rate for a revision hip replacement is 3 times higher than for an initial hip replacement.4Wolf BR, Lu X, Li Y, Callaghan JJ, Cram P. Adverse outcomes in hip arthroplasty: long-term trends. J Bone Joint Surg Am. 2012 Jul 18;94(14):e103. PubMed PMID: 22810410; PubMed Central PMCID: PMC3392201. This difference may be because:
- Patients tend to be older and therefore more likely to have other conditions, such as heart disease and type 2 diabetes, that put them at greater risk for a medical complication (such as a heart attack, blood clot, or kidney damage) during or following the surgery.
- Progressive bone loss, scar tissue, and compromised muscle function and quality increase the risk for complications such as infection, mechanical loosening of implants, nerve damage, and/or dislocation.
Revision surgery is more technically challenging than an initial hip replacement, and recovery from revision surgery may take longer and be more difficult for the patient.
See Post-Surgical Hip Replacement Precautions and Tips
Deciding When to Have Hip Replacement
Some people with moderate to severe hip arthritis will postpone an initial hip replacement surgery for many years in hopes of avoiding an eventual revision surgery. This concern is valid. However, there is evidence1Carol A. Mancuso, Jennifer Jout, Eduardo A. Salvati, Thomas P. Sculco; Fulfillment of Patients' Expectations for Total Hip Arthroplasty. The Journal of Bone & Joint Surgery. 2009 Sep;91(9):2073-2078. that post-surgical expectations are most likely to be met in patients who—
- Are younger
- Have a lower body mass index (BMI of 35 or less)
- Have better hip function and fewer symptoms before surgery
- Are employed
These factors indicate that patients may benefit from scheduling hip replacement surgery before hip arthritis pain:
- Becomes disabling and forces dramatic changes in daily routines and/or
- Affects other body parts, such as the low back, knee, or ankle, which may develop problems due to overcompensation
People of all ages can benefit from hip replacement surgery. A patient should talk to their doctor about the best time to schedule hip replacement surgery.
- 1 Carol A. Mancuso, Jennifer Jout, Eduardo A. Salvati, Thomas P. Sculco; Fulfillment of Patients' Expectations for Total Hip Arthroplasty. The Journal of Bone & Joint Surgery. 2009 Sep;91(9):2073-2078.
- 2 Harkess, JW and Crockarell, JR Jr. Arthroplasty of the Hip. Campbell’s Operative Orthopedics, 13th edition. Philidelphia, PA. Elsevier, 2017: 167-321.
- 3 Bayliss LE, Culliford D, Monk AP, et al. The effect of patient age at intervention on risk of implant revision after total replacement of the hip or knee: a population-based cohort study [published correction appears in Lancet. 2017 Apr 8;389(10077):1398]. Lancet. 2017;389(10077):1424–1430. doi:10.1016/S0140-6736(17)30059-4
- 4 Wolf BR, Lu X, Li Y, Callaghan JJ, Cram P. Adverse outcomes in hip arthroplasty: long-term trends. J Bone Joint Surg Am. 2012 Jul 18;94(14):e103. PubMed PMID: 22810410; PubMed Central PMCID: PMC3392201.

