Both gout and pseudogout cause sudden joint pain, swelling, and redness, making the two diseases difficult to tell apart. Understanding what makes each condition unique can help when diagnosing, treating, and preventing flare-ups, ultimately minimizing permanent joint damage.
Pseudogout is also known as acute calcium pyrophosphate crystal arthritis (acute CPP crystal arthritis). This page describes four ways gout and pseudogout are different.
1. Joints affected
Gout attacks typically affect only one joint.1Ragab G, Elshahaly M, Bardin T. Gout: An old disease in new perspective–A review. J Adv Res. 2017. Sep 1;8(5):495-511. PMCID: PMC5512152 DOI: 10.1016/j.jare.2017.04.008 In contrast, pseudogout attacks commonly affect between 1 and 4 joints.2Slobodonick A, Toprover M, Pillinger M. Crystal Arthritis. In: Efthimiou P, ed. Absolute Rheumatology Review. Springer Nature Switzerland AG; 2020; chap 15. Accessed September 15, 2020. https://doi.org/10.1007/978-3-030-23022-7_15 In addition, the locations of the flare-ups tend to differ:
- Gout most commonly affects the big toe, instep, heel, ankle, and/or knee.3Sidari A, Hill E. Diagnosis and Treatment of Gout and Pseudogout for Everyday Practice. Prim Care. 2018;45(2):213-236. doi:10.1016/j.pop.2018.02.004 About 50% of first-time gout attacks in men involve a big toe joint.2Slobodonick A, Toprover M, Pillinger M. Crystal Arthritis. In: Efthimiou P, ed. Absolute Rheumatology Review. Springer Nature Switzerland AG; 2020; chap 15. Accessed September 15, 2020. https://doi.org/10.1007/978-3-030-23022-7_15 In women, who are significantly less likely to develop gout, an attack is most likely to involve a knee.2Slobodonick A, Toprover M, Pillinger M. Crystal Arthritis. In: Efthimiou P, ed. Absolute Rheumatology Review. Springer Nature Switzerland AG; 2020; chap 15. Accessed September 15, 2020. https://doi.org/10.1007/978-3-030-23022-7_15
- Pseudogout is most likely to affect the knee, wrist, and/or large knuckles of the hand (metacarpophalangeal joints). It may also involve the hip, shoulder, and/or spine.2Slobodonick A, Toprover M, Pillinger M. Crystal Arthritis. In: Efthimiou P, ed. Absolute Rheumatology Review. Springer Nature Switzerland AG; 2020; chap 15. Accessed September 15, 2020. https://doi.org/10.1007/978-3-030-23022-7_15,4Genetic and Rare Diseases Information Center, National Institute for Advancing Translational Sciences. Chondrocalcinosis 2. Last updated January 12, 2018. Accessed August 4, 2020. https://rarediseases.info.nih.gov/diseases/1292/chondrocalcinosis-2 Unlike gout, pseudogout rarely affects the big toe.2Slobodonick A, Toprover M, Pillinger M. Crystal Arthritis. In: Efthimiou P, ed. Absolute Rheumatology Review. Springer Nature Switzerland AG; 2020; chap 15. Accessed September 15, 2020. https://doi.org/10.1007/978-3-030-23022-7_15
While certain joints are more likely to be affected, both gout and pseudogout can affect any joint in the body.
See Gout Symptoms and Pseudogout Symptoms
2. Causes
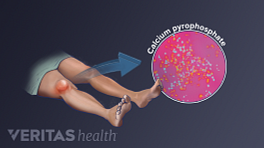
Gout and pseudogout are both caused by microscopic crystals that collect in a joint and trigger inflammation, which causes pain. The types of crystals are different:
- Gout is caused by monosodium urate crystals, often referred to as uric acid crystals.
- Pseudogout is caused by calcium pyrophosphate dihydrate crystals, often referred to as calcium pyrophosphate crystals (CPP crystals).
Not everyone who has urate crystals or CPP crystals in a joint will experience inflammation and pain. Researchers do not fully understand why these microscopic crystals lead to painful flare-ups in some people but not others.
See Gout Causes and Risk Factors and Pseudogout Causes
3. Severity, timing, and duration of pain
While gout and pseudogout can cause notable joint pain without warning, the severity of pain, when it appears, and how long it lasts may differ:- Gout pain is known to be excruciating and tends to be more severe than pseudogout pain.2Slobodonick A, Toprover M, Pillinger M. Crystal Arthritis. In: Efthimiou P, ed. Absolute Rheumatology Review. Springer Nature Switzerland AG; 2020; chap 15. Accessed September 15, 2020. https://doi.org/10.1007/978-3-030-23022-7_15
- A gout attack often strikes in the middle of the night. Pseudogout may flare up at any time of day.
- If left untreated, gout attack symptoms will usually go away within a few days or weeks. Left untreated, an episode of pseudogout can last days, weeks, or even months.2Slobodonick A, Toprover M, Pillinger M. Crystal Arthritis. In: Efthimiou P, ed. Absolute Rheumatology Review. Springer Nature Switzerland AG; 2020; chap 15. Accessed September 15, 2020. https://doi.org/10.1007/978-3-030-23022-7_15
Even though gout and pseudogout flare-ups will go away on their own, treatment is encouraged. Joint damage is more likely to occur without treatment.
See Pseudogout Treatment and Gout Treatment
4. Tendon involvement
People with pseudogout are more likely to have a build-up of calcium deposits in the tendons of the affected joint.5Miksanek J, Rosenthal AK. Imaging of calcium pyrophosphate deposition disease. Curr Rheumatol Rep. 2015;17(3):20. PMID: 25761927 doi: 10.1007/s11926-015-0496-1 These deposits are called calcifications. Tendon calcifications can occur because the crystals that cause pseudogout—calcium pyrophosphate dihydrate crystals—contain calcium.
Calcifications can be seen on x-rays as thin lines that run in the same direction as the tendon. Tendons that have undergone calcification may be inflamed and painful.
People with gout can have deposits of uric acid crystals in tendons. These deposits can be detected by certain types of imaging tests, such as musculoskeletal ultrasound.6Pascart T, Lioté F. Gout: state of the art after a decade of developments. Rheumatology. 2019; Jan 1;58(1):27-44. PMID: 29547895 DOI: 10.1093/rheumatology/key002 Uric acid crystal deposits or too much uric acid in a tendon may lead to inflammation and/or damage to the tendon (tendinopathy),7Andia I, Abate M. Hyperuricemia in Tendons. Adv Exp Med Biol. 2016;920:123-32. doi: 10.1007/978-3-319-33943-6_11. PMID: 27535254 DOI: 10.1007/978-3-319-33943-6_11,8Ray K. Crystal arthritis: Tendon damage in gout--a role for MSU crystals? Nat Rev Rheumatol. 2014 Jun;10(6):321. doi: 10.1038/nrrheum.2014.65. Epub 2014 Apr 22. PMID: 24752181 DOI: 10.1038/nrrheum.2014.65 which can be painful.
Both gout and pseudogout are treatable conditions. People who suspect they have gout or pseudogout are advised to seek a definitive diagnosis confirmed by medical imaging and lab tests.
Learn more
- 1 Ragab G, Elshahaly M, Bardin T. Gout: An old disease in new perspective–A review. J Adv Res. 2017. Sep 1;8(5):495-511. PMCID: PMC5512152 DOI: 10.1016/j.jare.2017.04.008
- 2 Slobodonick A, Toprover M, Pillinger M. Crystal Arthritis. In: Efthimiou P, ed. Absolute Rheumatology Review. Springer Nature Switzerland AG; 2020; chap 15. Accessed September 15, 2020. https://doi.org/10.1007/978-3-030-23022-7_15
- 3 Sidari A, Hill E. Diagnosis and Treatment of Gout and Pseudogout for Everyday Practice. Prim Care. 2018;45(2):213-236. doi:10.1016/j.pop.2018.02.004
- 4 Genetic and Rare Diseases Information Center, National Institute for Advancing Translational Sciences. Chondrocalcinosis 2. Last updated January 12, 2018. Accessed August 4, 2020. https://rarediseases.info.nih.gov/diseases/1292/chondrocalcinosis-2
- 5 Miksanek J, Rosenthal AK. Imaging of calcium pyrophosphate deposition disease. Curr Rheumatol Rep. 2015;17(3):20. PMID: 25761927 doi: 10.1007/s11926-015-0496-1
- 6 Pascart T, Lioté F. Gout: state of the art after a decade of developments. Rheumatology. 2019; Jan 1;58(1):27-44. PMID: 29547895 DOI: 10.1093/rheumatology/key002
- 7 Andia I, Abate M. Hyperuricemia in Tendons. Adv Exp Med Biol. 2016;920:123-32. doi: 10.1007/978-3-319-33943-6_11. PMID: 27535254 DOI: 10.1007/978-3-319-33943-6_11
- 8 Ray K. Crystal arthritis: Tendon damage in gout--a role for MSU crystals? Nat Rev Rheumatol. 2014 Jun;10(6):321. doi: 10.1038/nrrheum.2014.65. Epub 2014 Apr 22. PMID: 24752181 DOI: 10.1038/nrrheum.2014.65